Transcript
This transcript was automatically generated and may contain minor errors or inaccuracies.
Joe Moore: [00:00:00] Hi everybody. Joe here with Kyle. How are you doing today, Kyle?
Kyle Buller: Pretty good, Joe. How are you doing? It’s, uh, been a while since we’ve done one of these.
Joe Moore: It’s, um, not fair to us or the, or the world, so I’m glad we’re finally doing it.
Kyle Buller: Yeah.
Joe Moore: Um, yeah, so, um, today we get a lot to chat about.
Joe Moore: We wanna chat about like our community platform, breath work that’s coming up, uh, this weekend. And, um, probably some news items that are gonna be worth discussing too. So yeah, very excited to get into all of it. Um, yeah, and I guess congratulations to us and, um, for graduating Vital Cohort four. Just, uh, was it this past Sunday?
Kyle Buller: Yeah, this Sunday, cohort four. So if you’re chiming in here, congrats. And yeah, it’s been a journey, so yeah, it’s been been awesome.
Joe Moore: It’s really, really cool, um, to have finally been a part of a [00:01:00] graduation. Like I saw you and the rest of the team do it. I’ve, you know, popped in and watched a little bit, but like Vital, vital was kind of traditionally yours and like I backed off.
Joe Moore: So it was like really cool to kind of see that and, um, participate and, uh, yeah, it was just, you know, an, a very great experience for me. How was it for you?
Kyle Buller: You know, cried a whole bunch as as usual. Um, which is always pretty funny. I never always think I’m gonna get that emotional. But, um, yeah, it’s just, I think just like the connections that we make in the program, um, it just so heartfelt.
Kyle Buller: Um, so yeah, it was, it’s always really nice to, you know, it’s sad and nice to know that people are now out there in the world and hopefully, you know, showing up in their communities in whatever way that they feel like they, they wanna show up, whether they’re educating or doing harm reduction integration, hosting retreats, just creating spaces for other people.
Kyle Buller: Um, it’s, it’s just really nice that we, there’s a lot of people [00:02:00] out there doing really awesome work, but yeah. How was it for your first time?
Joe Moore: Um, it’s kind of like emotionally overwhelming to just know that we’ve been able to help people. Um, kind of unfold who, who they want to be in the space, you know?
Joe Moore: Yeah. And just do like the adventure of self-discovery around their, you know, psychedelic future and how they want to show up and where they, what they want to do. And yeah, it was just really, really amazing ’cause it is so meaningful to people to be able to, you know, feel competent enough to share this stuff in, in helpful and safe ways.
Joe Moore: And, um, yeah, I just, I was pretty overwhelmed, honestly. And I’m just really grateful for everybody, you know, sticking with us. Yeah. Yeah. So, um, yeah, like how do you, so I guess like, not everybody listening knows all, everything about Vital, right? Like, it’s our world, so we assume it, but how do you, how do you like to talk about vital these days?
Joe Moore: Like, what is it? [00:03:00]
Kyle Buller: Yeah, I feel like it’s like shifted a whole bunch in, in ways. Obviously, you know, it’s been, um, pretty consistent where I’d say, you know, it’s our 12 month training program and psychedelic informed practice harm reduction integration. Um, so, you know, getting people really spun up on, you know, how to support people that are having psychedelic experiences, whether it’s on the, the prep side, um, for those that are, you know, doing stuff in the underground and decrim areas, really getting spun up on all the ethics of space holding and, and all that, uh, stuff.
Kyle Buller: And then the integration. But I also over the years, have felt like it’s just more than that. Um, it’s really turned into a community. Um, and I feel like that’s been a very large focus of vital is the community aspect of it. Um, really cultivating the relationships, cultivating the community between cohorts, um, and, you know, thinking about.
Kyle Buller: Like some of our [00:04:00] experiences in in Dream Shadow with that being a community. I think about like my time at Burlington College, it was a very community oriented program where it was just also beyond just learning. It was really about, it’s really about the connections that you’re starting to make with folks.
Kyle Buller: And so in some way, I feel like that is essence of vital, is it’s really community focused. Um, and I hope that shines through and it does, it does seem like that, um, with all the students that, that come through the program and all the touch points that we have too, right? Like we have like little meetups.
Kyle Buller: We do. Webinars on Mondays where some of the alumni come back and present on topics. We also have another group where we just have discussion groups that are a little bit more informal just for cohorts to mix and mingle and, and have discussion and learn from one another. So it’s, yeah. It’s also, I think, beyond just the theoretical learning aspects of it and really trying to foster that community so we can all lean on each other, um, as we always like to say, we can’t do this work alone and we [00:05:00] need people.
Kyle Buller: And so, um, I feel like that’s where, um, vital really kind of shines through.
Joe Moore: Right? Yeah. I think in a lot of ways we were trying to bring forward what we got at Dream Shadow and give people similar opportunities for kind of connection and, um, kind of, uh. It’s funny, right? Is it, is it a non-directive approach?
Joe Moore: Is it not? It’s kind of like a little bit of both. Um, yeah, and I think about that in the psychedelic container too. It’s like, is that really non-directive or is it Right. You know, a mix of growth. Exactly. Is it? Yeah. Right. It’s, it’s kind of like a scaffolding and we help you kind of climb through it and navigate your way through it.
Joe Moore: And, um, yeah. So where do you want to be in the space? Like, you could be anywhere you’d like, the, the rules right now are not very firm. Um, there’s certainly some legal consequences and we make sure to include a lot of those in our education. So, you know, be careful and be safe, everybody, but you know, there’s also edges.
na: Mm-hmm.
Joe Moore: Yeah. Edges are where the most [00:06:00] interesting stuff happens. I think
Kyle Buller: that is true. And yeah, you know, we, I think anybody getting involved right now, like we are, everybody’s kind of pioneer on the forefront, right? Like the things are just getting developed and so it is confusing to try to navigate like, where’s my place?
Kyle Buller: How do I show up? What do I do? Um, as like a new field is emerging. Um, and, you know, people that leave vital go through, you know, a lot of people don’t end up doing any sort of facilitation, right? They, I’ve heard this multiple times. They’re like, you know, going through this program has taught me a lot and taught me like, maybe I don’t want to do this right now.
Kyle Buller: I need to learn more. Like I’m more interested in. The harm reduction and integration aspect, or I’m really interested in just creating community groups and being an educator, um, and, you know, stuff like that. And so, you know, it’s been really cool seeing, um, a bunch of our students go out there in the world and, and do stuff.
Kyle Buller: Like at psychedelic science was really nice. There was like, I think four students that had booths there. [00:07:00] Um, and they’re all kind of showing up in their own ways, whether they’re promoting like their retreat center or they’re offering education offerings in, in different, uh, like their, in their specialties.
Kyle Buller: So yeah.
Joe Moore: Yeah, that was definitely a really special feature, um, for us, I think, to seeing the success and the, the being out there in the world. Not even necessarily financial success, because that’s like, not necessarily primary, but just the fact that you’re out there in the world and active in the thing that you really wanted to be active in and, and contributing.
Joe Moore: Yeah. Yep. Yeah. So, um. Yeah, if folks wanna learn more vital psychedelic training, we don’t have our dates firmed up yet. Um, vital psychedelic training.com. We can learn more about it there. Um, what can we say about it publicly at this point, Kyle? I don’t, I don’t think we have all that much we can say,
Kyle Buller: yeah, we don’t have the dates yet, but we are looking at either like May or September, just trying to figure out some scheduling things.
Kyle Buller: So, um, if you are interested, you can just go to the [00:08:00] website and then, um, you know, you could put an application in or sign up for, uh, emails just so we can stay in contact. Um, but yeah, we’re just ironing out a few details for our cohort. Six, if you are interested in, in joining. Yeah.
Joe Moore: And then, um, let’s talk about what’s going on this weekend.
Joe Moore: We have, uh, we’ve been kind of pushing for a while to, uh, market our, uh, three day, I guess two day two two day plus, um, breath work, workshop, dream shadow, transpersonal breath work, kind of a graph style, breath work method that we learned, a dream shadow. Um, what do we wanna say about that?
Kyle Buller: We have that coming up and it feels really good to be offering, um, breath work again.
Kyle Buller: Um, felt like I took a little hiatus after some of the vital retreats. Um, but yeah, we have this, uh, weekend workshop coming up Friday to Sunday up here in Breckenridge. So anybody’s listening that’s in the Colorado area that wants to come up for the weekend to do some breath work, we do have some spots open.
Kyle Buller: Um, so it’ll be fun. And it’s [00:09:00] beautiful up here right now. Leaves are popping. There’s snow on the peaks. Um, it’s a really beautiful time of year to come visit. Yeah,
Joe Moore: so pretty right now. Um, yeah, and I think our last workshop was just like so good for us, uh, for others too, but really primarily like we did.
Joe Moore: We, I would have really, I think, really good feelings about it and just was so good to be back in the saddle again after such a while.
Kyle Buller: I was gonna say you, that was like a first workshop for you in a number of years, right?
Joe Moore: Like, I don’t know that I. Really facilitated a full on like two part breath work session since before COVID.
Joe Moore: I might be wrong, but like I don’t, yeah, I haven’t really been in it for a bit and it felt really great to be back. Yeah. Thank goodness. Yeah. Yeah. Um, yeah, just, you know, the thing that I know really well, um, and I’m comfortable in that space and it was just, you know, good to be there and definitely good to be with you.
Joe Moore: [00:10:00] Uh, learned a bunch from you on the somatic front, um, which is great.
Kyle Buller: Yeah. Yeah. Minus the little bit of the, the music hiccups here and there.
Joe Moore: Right. Nobody noticed it sounds like they didn’t tell us they noticed at least. But you know, the idea is like, there’s, there’s a lot of, um, things to know about music and, and breath work and psychedelic sessions like, um.
Joe Moore: There’s so many possible points at which equipment can have issues and we want to kind of like work towards, you know, how can our systems be really kind of bombproof, but also have a backup.
Kyle Buller: You’re always thinking about that. And like, I think about it a little bit here and there, ’cause I’ve never had any like big hiccups, but like, how do you think about like, music backup and like psychedelic and breath work sessions where it obviously plays a really important role, um, in one’s experience.
Kyle Buller: So like those hiccups can also really cause a little bit of like, I don’t know, confusion with folks where all of a sudden the music stops and you’re in it, or there’s weird [00:11:00] like, artificial artifact noise coming through and you’re like, what the hell is this?
Joe Moore: Right? So like we can kind of name that we use this kind of like audio processor, um, because the outputs from a laptop aren’t really like producing like the, the most rich audio.
Joe Moore: Um, and so like. It’s never failed before in years and years. So we, we had a failure. I didn’t really check the stars to see if there was something up there, but maybe, and then, um, it was, it was kind of felt really glitchy and like digital weirdness was going on and we just didn’t know what to do and we had a hard time kind of solving that, um, in real time.
Joe Moore: Oh yeah, that was like the most intense kind of, um, music failure I’ve been a part of, which is fascinating. I’m glad we were able to do it together. Um, but like Lenny talks about having like a, like a generator backup at his house for audio. Um, worst case you can put on a little boom boxy thing. Um, I like, I like to have [00:12:00] multiple different kind of things, so, you know, a little Bluetooth speaker, like I have this little small little Bose thing.
Joe Moore: That’s nice. Um, and then, uh, you know, typically we’re using like a relatively big size PA system. I, I personally have like three different. Oh, geez. If we put in the, like the DJ control, there’s like five different mixers that could be used for that kind of a situation that we do. Um, and I bring two at least.
Joe Moore: Um, so if one fails, we can flip over to the other. Sometimes that gets stressful though. Um, and then like any, any individual piece can fail, um, at any point. And there’s no way to really tell, just like, you know, hard drives used to explode all the time, right. And we could never tell. And how much music have we lost as a result of that crap?
Joe Moore: Tragic. Um, yeah. And, uh, yeah, then, you know, can you, can you have a backup? Like, historically, I never thought, like [00:13:00] my DJ equipment at the mixer and beyond like speakers and, and all that would fail. But they, they can, so what I would do historically is I would have the, um, a PC playing a Wave file. So there’s like very little happening, um, like wave, like there’s not really much computing required ’cause there’s not much compression, there’s not any compression really.
Joe Moore: So like the computing power should be really small. Um, and I use an app that hasn’t really ever failed on me, like VLC. Mm-hmm. Um, really popular media player. Um, and that’s like really low computing requirements as well. I think it’s even open source, which is, yeah, it’s pretty lightweight. Yeah. And then, um, I’ll have secondly a audio device into two other channels that’s actually playing in real time, a playlist.
Joe Moore: Um, it could be my breath work playlist. Could be something else. Could just be a track on loop. Um, and so if the audio on like channels one and two start failing, I bring up three and four from my phone or [00:14:00] iPad or whatever it is. And then, um, there’s very little loss, um, of like time. With music, with the, with the people breathing.
Joe Moore: So I think like that’s how I historically did it, but now that maybe the mixers are, sorry, are failing, and like how do we, yeah. How do we actually understand like what part of the equipment’s failing? Um, so you kind of have to like be somewhat technical, somewhat competent with your equipment. So that’s why maybe don’t overcomplex, uh, make it too complex at first.
Joe Moore: Yeah. Um, start simple and build and stay comfortable with your gear. Um, yeah. So I don’t know, did you, did you have any kind of like takeaways.
Kyle Buller: Um, well, I think like testing your gear out. ’cause that was the first time I used my laptop, I think, on that mixer or the output with all those speakers. And like, I’ve never had an issue with like that weird digital artifacting that came through.
Kyle Buller: Mm-hmm. And so I wonder if it was like more power or something that was sucking out of the computer, [00:15:00] um, or computer needing to, to do more. Um, but, you know, I think I always will. So I, I typically use like flack files and I use a program called Mix. So I’m able to like auto DJ and like real time, like mix things in case
Joe Moore: Slack doesn’t have compression either, like Right.
Joe Moore: Yeah. It’s like really light. Or maybe it does have compression, but it’s really light. Yeah.
Kyle Buller: And then, um, yeah, ’cause sometimes I like to mix live. Like there’s the songs coming up and I’m like, eh, it’s not really gonna fit here. I kinda wanna switch it up and, or I notice like, you know, things maybe I need to add something.
Kyle Buller: Um, so I always. We will create a duplicate of that on Spotify. And so that’s what we ended up doing. It’s like, thankfully I had that, um, on Spotify as well, so we could just switch over, um, as like we were starting to have some of those weird digital artifacting hiccups there in the middle of a session.
Kyle Buller: Um, so yeah, I think always having a backup, um, is really [00:16:00] important, um, when, when you’re doing this stuff. But yeah, testing, testing all the equipment first. Like I think we didn’t do extensive tests with it beforehand. Um, no. And so that was like really the first time, like running my computer on, on a system like that.
Kyle Buller: We should check it
Joe Moore: again tomorrow. Yeah. What I realized is we could actually use like headphones like this Yeah. Um, to actually have a, like simulate that like kind of say, is it the output from this? Or, ’cause we didn’t, I don’t think, had earbuds even to plug in and check. Yeah, yeah. No. Yeah. And it’s, you know, it’s complicated and generally folks, you’re not gonna have a problem.
Joe Moore: When you do you want to have a plan, like exactly the equipment, exactly. Like these days it’s really solid. Like Windows doesn’t really crash all that much anymore. Mac doesn’t really crash that much anymore. Um, there’s types of devices that crash even less like a, like a real DJ mixer. Like if we throw up like my big DJ controller and plug in a USB and play, [00:17:00] like these things are designed to play big festivals and the stability is crazy.
Joe Moore: Like, yeah. Um, even Skrillex’s laptop has crashed when he is playing live. So like that’s kind of probably have a backup computer though. Right, right, right. What do we have three computers there? Yeah. Which is nuts. Which is really crazy. Um, and we still couldn’t like figure out what was going on. Oh, what was it?
Joe Moore: No, my, one of my laptops just wasn’t producing audio outta the headphones port. Um, the other one I think had some weird issues too. It was a really surreal experience, but I’m glad we got to the other side. Yeah. I don’t
Kyle Buller: think I’ve ever had that many, like tech hiccups, like doing music stuff and I think it was a good lesson learned of like, yeah, prep all your stuff, like test it out, make some like backup plans.
Kyle Buller: And then as I switched over to my phone too, I was like also thinking. Oh, I’m not connected to the wifi, so I can’t like, go into like airplane mode to like cancel any calls. If this is streaming from my phone on Spotify, if a call comes through, it’s gonna [00:18:00] disrupt the music. And like, so then I was like kind of panicking, like, oh man.
Kyle Buller: Yeah. What if like a call comes through like as we’re streaming this through the phone, that’s gonna be really disruptive. Mm-hmm. Um, so it’s like all these little things you don’t think about. And then yeah, you need to like be on your feet real time to try to problem solve so it’s not so disruptive to, to folks.
Joe Moore: Yeah. And take notes here. There’s a lot of really good gems here that you, you know, learn from our mistakes. We make the mistakes so you don’t have to. Mm-hmm. Um, and I think, uh, do not disturb, uh, mode sometimes works, but sometimes the song will interrupt and you don’t actually know until you test it and like, do you actually ever really know?
Joe Moore: Um, ’cause these things update and like software changes every day, so you don’t know really how it’s gonna play. Um, so be careful out there. That’s why I liked the, um. The old school iPods were really great, um, with the hard drive and you can just kind of plug right in and that was lovely. Um, but you know, there’s limited limitations [00:19:00] there.
Joe Moore: Yeah. Obviously our files were like, my playlist, it’s like three to five gigs. ’cause it’s a wave file, it’s giant. So like it could even fill up those, those things. Um, yeah. But yeah, the sematic work that we got to do there, the, the kind of group processing work that we got to do there, the group bonding, like I think the group’s still talking to each other, which is amazing.
Joe Moore: Mm-hmm. Um, we, we heard that they got to together and did like a party in the front range, which was really cool. So it’s just like lovely to see that. A workshop like this that, you know, we believe in this format quite a bit. I think so. You know, just seeing it again and again and again. Workout. Great. It’s just always so reassuring.
Kyle Buller: Yeah. Yeah. It’s nice to just be able to share it with folks too. Um, yeah. ’cause how impactful has it been in our lives? Right. Just to be able to like, share it with other folks. Mm-hmm. It’s really nice, really special.
Joe Moore: Yeah. So, um, that’ll be coming up Friday, so tomorrow. So [00:20:00] if anybody’s in Colorado wants to join us, rec breath.com or psychedelics today.com/events, you can learn more.
Joe Moore: Um, we’d love to have you still time and, uh, what else is going on? Um, yeah, we’re trying to launch a kind of membership site here to get people, um. Kind of a little bit more active in our community. Like we’ve had this kind of, um, online Facebook alternative. It’s just us, uh, for a bit now, and it’s been great.
Joe Moore: It’s mostly vital folks. Um mm-hmm. And there’s some patrons in there. I think we have 33 paying patrons is what I saw the other day in the, in that platform. And that’s been really fun, um, to see that and really helpful for us. So thank you everybody that’s participating like that. It helps a lot. Yeah. Um, and yeah, we’re trying to figure out what do folks want.
Joe Moore: I think we’re gonna bring in, um, exclusive content, hopefully figure out ways to include courses, maybe some courses that we’ve had out for a while. And, and I think what, we have five courses in development right now that might be [00:21:00] included there. So, you know, stay tuned. Um, and we’d, we’d love and need your support.
Joe Moore: Um, but yeah. Kyle, what are you excited about about this community platform?
Kyle Buller: I’m excited just to like, yeah, you know, we’ve had this, um, and just to like really engage with it a little bit more. So like having kind of like exclusive live streams like this, doing more of it. Um, also, uh, I. Book clubs, like those are always really fun to just like get together and like talk about material that way.
Kyle Buller: Um, so yeah, I just feel like, you know, we’ve been really engaged in the vital community for the past few years. Um, hence why like, I don’t really podcast as much as I used to. Um, but yeah, really excited to just gauge the engage, like the, the larger audience, our, our whole PT audience here. So, um, yeah, it feels like we’ve been very kind of like focused on the vital community and um, yeah, now trying to um, open it up, you know, I think we’ve learned a lot through that and like creating [00:22:00] that and then just being able to open it up, um, to outside of folks that yeah, vital might not be a great fit for Right.
Kyle Buller: It’s a, it’s a pretty big, um, it’s a pretty big commitment and yeah, I’m seeing David there in, in real life events for sure. Yeah, that is part of the plan too. We wanna do more in person events for the community. It’s really, I love this overlay.
Joe Moore: Yeah. Um, for sure we’re, we’re working on, um, in-person events more regularly.
Joe Moore: Um, I’m traveling a bunch in the near term, so I’m hoping to say hi to folks in the northeast, like Philadelphia. Um, Boston. There’s a chance New York, but I’m not sure. It’s a kind of logistically complicated, but if anybody wants to help me in New York, reach out, I would love that. Um, but yeah, just getting together, even if it’s for a short meal or sandwich or whatever.
Joe Moore: Amazing. Um, I want to do bigger. More robust events, especially for the vital community. But you know, that takes resources and time. So the more support we get [00:23:00] here, um, in our community platform, the more we can, um, spend our time actually developing those in-person events to mm-hmm. You know, bring value and, and, you know, community and much more.
Kyle Buller: But having a lot of these conversations lately just around like how we’re just entering this age of like high tech and AI and um, yeah, we can channel Northern California for you as well, David. Um, but, uh, yeah, just how important it is. Like, I was just chatting with somebody I think last night, um, just how.
Kyle Buller: You know, community is gonna get us through, um, you know, some challenging times. And I think again about like going through some challenging times and having like the dream shadow community there for me and for everybody else. Um, but yeah, like as you know, we just kind of enter this like crazy digital world, um, where yeah, everything feels like really artificial.
Kyle Buller: Like yeah, being able to come together, um, in person online, to like really, um, you know, cultivate, uh, [00:24:00] human relationship. I think it’s gonna be really, really important as we progress into the AI age of whatever the hell it’s gonna bring to us.
Joe Moore: So, you know, that’s an interesting point. Like, I, I think we should name, um, dead internet theory.
Joe Moore: By way, David, I’ll, I’ll be, I’ll be in, uh, San Francisco, November 7th for the Heroic Heart Gala. Uh, maybe we could hang out before, after that. Anyway, the, um, the idea is that as more and more content becomes generated by ai, it’s, it becomes somewhat recursive and problematic in that, um, the data that’s getting cited is actually bad data.
Joe Moore: ’cause it was generated previously by ai, by AI and Misattributed. So there’s becoming this like, really scary problem. And, um, at a certain point, at what point does the internet become totally not useful, um, or at least radically less useful? Um, you know, in situations like [00:25:00] this, you know, we’re, we’re still doing okay because we’ve read a bunch of books and lived a lot of life, um, and, and know a lot of folks.
Joe Moore: Um, but yeah, like who’s to say Wikipedia is even gonna be all that helpful in a handful of years. Once, um. AI has had its way with Reddit and like the citations get really, really complicated. Yeah. So in-person, community is gonna be really important. Getting to know people and trusting people. I, I hope folks like us can still, you know, maintain some sort of sense of truth and, and help everybody cut through the bs.
Joe Moore: Mm-hmm. Um, but yeah, I don’t know. What do you think?
Kyle Buller: Uh, I’ve been listing revisiting like Terrence McKenna, um, over the years. Um, or not over the years, over the past, like month or so, because I remember years ago I heard him talk about, um, this archaic revival and he was talking about how in the future people are gonna just be living in their own little worlds and that there’s gonna [00:26:00] be the computer chip behind the eye.
Kyle Buller: Um, and we’re gonna be interfacing pretty much with like augmented reality, like through like a, an implant like that. Um, and. Then, you know, there’s that whole announcement of like the meta glasses coming out and it’s not too far off. And like I just, I, I think that it, it’s just really interesting to hear Terrence talk about this stuff in the nineties.
Kyle Buller: Um, and kind of like just, you know, and Terrence had all sorts of crazy ideas, but it’s like, I feel like we’re getting closer to like what he was actually like, you know, talking about back then. Um, and I just always come back to like his, I think it’s like titled his last interview where he is just like, it’s just gonna get so weird that we just gotta talk about how weird it is.
Kyle Buller: Um, and I feel like we are hitting this point in, in human, human history where it’s getting pretty weird out there. It’s very psychedelic in a way. It’s like very confusing.
Joe Moore: Yeah, it is. It certainly is. And um. Again, having that kind of [00:27:00] community that can handle complexity and can handle stressful stuff and crisis with you and, and more is, is gonna be just increasingly important.
Joe Moore: So, you know, build that we can, you know, leverage our community with you. You know, you can join us. Um, but definitely build something locally for you too. Um, yeah. And yeah, whatever it is. Gardening club. Yeah. You know, seed swap, book club, whatever those local, yeah,
Kyle Buller: those local communities are really important.
Kyle Buller: You know, I think that helps with like resiliency when like, things are kind of like getting really shaken up. Um, so yeah. You know, have like your larger community, also have your local communities, um, and have a diversity of community. I think it’s, it’s really important. Um, I like Debbie’s comment here. I came for the psychedelic state for the community.
Kyle Buller: I always actually said that about like the breath work too. It’s like, came for breath work first, but ended up really kind of staying for the community and started becoming more about the people than, than the experiences.
Joe Moore: Yeah. Um, so. [00:28:00] I’ve seen a number of communities and they’ve, they’ve done interesting stuff.
Joe Moore: I, I think I started seeing Discord kind of explode with communities around that like NFT hype cycle a bunch of years ago, which is interesting. And just saw people kind of communicating in all sorts of interesting ways, not just about like magic internet money go up kind of stuff. Like it’s, you know, sharing news and memes and jokes and like, you know, there was a culture around some of them that was actually real as opposed to purely just kind of greed culture.
Joe Moore: Mm-hmm. Which was also there for sure too. But, um, it was just fun to see that and I was like, oh, okay. Like we can do something here. Um, and you know, I think in time we didn’t, I, I’ve always been a little kind of skeptical on discourse, like, that seems like just a little edgy to put psychedelic community because, you know, um, it’s somebody else’s servers.
Joe Moore: It’s not really all that, you know, they could shut you down. Um. And, you know, even our community, it’s not all the way private, right? Like it’s [00:29:00] hosted somewhere. So, you know, if you want to do hyper secret stuff, like the Internet’s probably not the best place for it, but it still doesn’t mean you can’t help each other and communicate.
Joe Moore: And then take it to signal if you need to, then take it in person if you need to. Um, and, you know, we’re here for kind of helping with that scaffolding. Mm-hmm. And, uh, you know, what kind of content do you need? What’s gonna serve you in the projects that you have going on? Not just like, you know, cool trip stories, which, you know, those are fun too.
Joe Moore: But also, you know, what are the helpful stories that are gonna help you build the thing that you want to build with people?
Kyle Buller: Yeah.
Joe Moore: Um, so we’re open to questions, so I think most platforms can ask questions, so please do. Um, yeah, I’d love to just kind of interact with you all, um, and see what’s going on out there for you and see what we can kind of like interact with, I think.
Joe Moore: Um, yeah, finally, just please check out our community, psychedelics [00:30:00] today.com/navigators. Um, we’re gonna be putting up all sorts of like, scaffolding there and higher level memberships with more access to us and, um, the community and, you know, just stay tuned for all that. Um, I think we’ll have that kind of announced in the next handful of days, hopefully.
Joe Moore: Yeah,
Kyle Buller: we’ll, we’ll be rolling it out over time.
Joe Moore: Yeah. So, um, let’s see, what else here? Um, what are the skills important to learn at the moment? Um, David to asks that question, I’ll put it up on the screen for everybody watching video. Um, so. It depends on where you’re at. Um, you know, I think, uh, I think understanding how, how you could get in trouble digitally is a really good one.
Joe Moore: So there’s that digital security class I’ve taught a handful of times. We’ll probably have that in the community in the near term. Um, if you want coaching or consulting on that stuff, I’m open to that just hit us up. Um, but the idea is like, how are you [00:31:00] exposing yourself and what are the actual risks? Um, are you covered legally?
Joe Moore: You know, are you actually working with lawyers appropriately? There’s so much to this. Um, and, uh, I don’t have a broad enough view into what every community is like in the psychedelic ecosystem, so I can’t really say. Do you, do you have any thoughts on, on to where he’s, uh,
Kyle Buller: yeah, and I, I’m kind of just taking that too, like what are important skills of like, the times?
Kyle Buller: Um, and one thing that comes to my mind is, uh. As you were kind of talking about like dead internet theory and like all this other stuff, it’s just like our discernment. Um, and really trying to get in touch with that a little bit more because, and you know, that’s also really relevant for psychedelics, right?
Kyle Buller: It’s like you get a message, do you necessarily believe it at face value right off the bat? Um, or it, um, you know, do you sit with it a little bit? And again, you know, now everything. I think we’re just entering this [00:32:00] like new age of like. Yeah, you see some videos and you’re like, is that real or is that ai?
Kyle Buller: You know, it’s like, it’s really hard to tell what’s true, um, anymore, which is like, kind of concerning. So I think like our just discernment is more important than ever. Like, you know, and also like, you know, what are we taking in like, ’cause obviously all this stuff like affects us on so many different levels.
Kyle Buller: So, um, yeah, like how are you, how are you taking in information? How do you discern information? Um, it’s all, I think, like, really crucial right now. Um, ’cause there’s a lot of noise out there in the world. Um, and there’s a lot of, lot of, a lot of weirdness as I guess Terrence would say.
Joe Moore: So much weirdness.
Joe Moore: Yeah. High weirdness moment. And yeah. David, if you’re talking, if David, if you’re talking about like survivability and like prepping, um. I’m not necessarily all that fluent on what’s going on today. I don’t know, um, [00:33:00] what to really say, but community is gonna help. Um, so getting together, I think, uh, in my permaculture class it was like, um, if you have a hundred people in your kind of circle with all the right skills, like you can kind of flesh out kind of a really great society.
Joe Moore: Um, and, you know, there’s specialist skills beyond that, but that’s where societies can keep interacting, uh, with each other. Yeah. Um, yeah, I like, I like the Chomsky, anco, cynicalist kind of model where it’s kind of like hierarchical unions that are kind of, um, voluntarily kind of associated and, and kind of cooperate too, so, mm-hmm.
Joe Moore: It’s important that groups kind of interact and negotiate skillfully and we kind of like decrease coercion over time. Hopefully. Hopefully. Um, because consent, uh, matters, I think. Mm-hmm. Um, yeah, definitely. I dunno if the government agrees still, but maybe. Um, so we’ll get there, get there in time. So just keep hope alive.
Joe Moore: Um, [00:34:00] and uh, yeah, so I think like what kind of news have you bumped into lately in the psychedelic arena, Kyle, that’s got you interested in, um, curious.
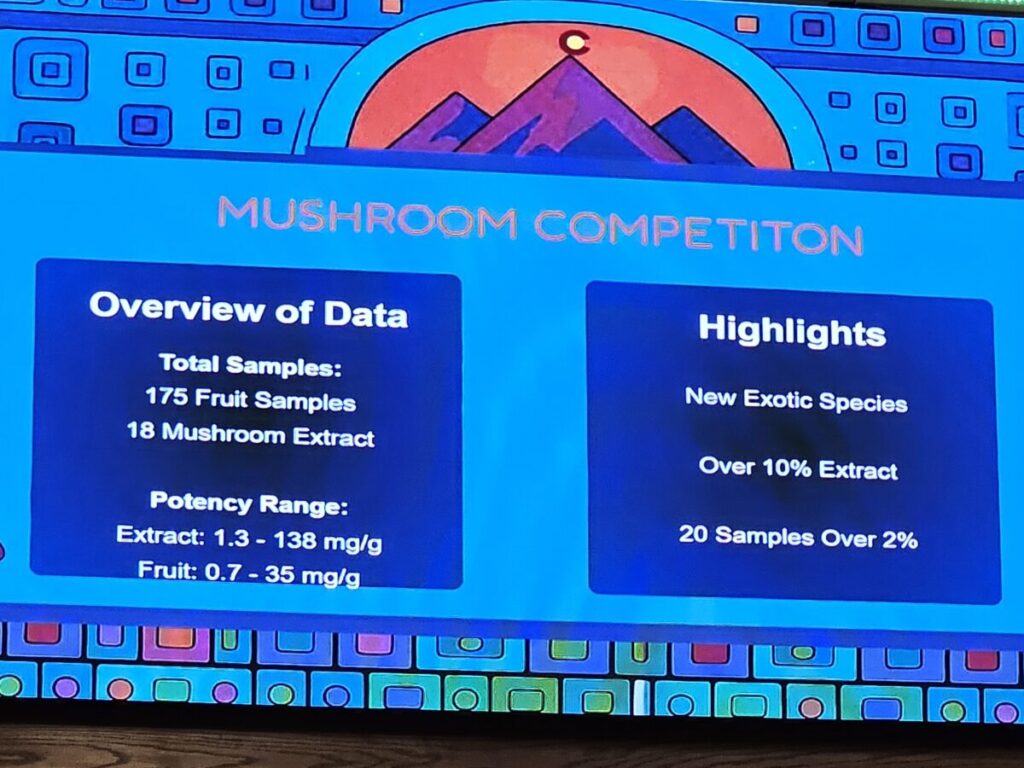
Kyle Buller: One I posted about maybe last week. Um, and, you know, maybe this also comes back to discernment as well, and, and what you’re consuming. Um, it was a study that was published, uh, in Oregon, um, surveying 11 different, uh, mushroom products.
Kyle Buller: Um, I think 10 of ’em were gummies. One of ’em was a chocolate bar. Um, but none of them contained psilocybin. Um, they came back with like all sorts of different other, uh, you know, ingredients. Uh, and you know, I think if we’re, you know, you’re talking about consent, um, having informed consent of like what you’re ingesting is super, super important.
Kyle Buller: Um, you know, some of them did contain psy. Um, you know, I feel like, you know, I think that that’s pretty legit. Psilocybin ilsy, right? Psilocybin converts into psilocin. But again, [00:35:00] it’s like, you know, do people know the dosing? Do people know what they’re ingesting? Um, and yeah, some of these products just didn’t have any sort of psilocybin or psilocin in it.
Kyle Buller: Um, most of, I think some, some came back with like THC kava, um, some of them were just functional mushrooms. Um, I don’t remember everything off the top of my head right now, but, um, you know, that is a bit concerning ’cause people just see these products and they go, oh, this is legit. Like, people are doing really good marketing.
Kyle Buller: Um, and then just not having good, uh, informed, you know, consent here around like, should I est this? Do I know what I’m taking? Um, and I actually, it’s, it’s such an interesting thing and I, I might have mentioned this like on a podcast a while ago, but. I was down in, um, I was down in Key West back in March and uh, after I went down there for a wedding and me and my friend decided to go down to Key West just to hang out for the weekend.
Kyle Buller: And, um, it was really interesting. There was all [00:36:00] these like hemp shops within like, I mean, there was just one after another after another, and a bunch of ’em had these signs that they were selling psychedelic mushrooms. And so I decided to pop in there and, um, see, hey, what, what’s going on here? And I asked the guy, I was like, Hey, like, what’s in these mushrooms?
Kyle Buller: He’s like, I can’t tell you. And I was like, what do you mean you can’t tell me? He’s like, uh, it’s a proprietary blend. I, I can’t tell you what’s in it. And I’m just like, well, that’s kind of sketchy. I was like, is it mus al? Like he is like, we don’t say that word around here. And I’m like, and I was like, I, you know, I was like, I work in the psychedelic industry.
Kyle Buller: I was like, I’m just like highly fascinated about like how you guys are like getting these workarounds or, or what’s actually in these, these, these bars and, and products. And he just told me he’s like. There’s a loophole that we’re able to get through that this is a food product and we’re able to just like label it as a proprietary blend.
Kyle Buller: Um, so I can’t like tell you what’s in it. I can just tell you it’s a proprietary blend, but it’s just like, again, informed consent. It’s [00:37:00] like, you know, you have no idea like what you’re ingesting. And I just think that, you know, it’s harmful. Like what if somebody has like, um, an adverse reaction and needs to go to the hospital and you can’t tell, like, you know, the doctors like what you just ate, you know?
Kyle Buller: Um, it’s like, oh, I ate this chocolate bar, this proprietary blend of mushrooms. Like I have no idea what I, I actually ingested here. Um, so, you know, be careful. There’s a lot of products out there on the market and they are showing up at like gas stations and head shops and stuff like that all throughout.
Kyle Buller: You know, the country. Um, and yeah, it does seem like there’s these like interesting workarounds, um, being food products, um, and you know, who knows what’s actually in it. So, um, you know, maybe try to find somebody that’s a bit trusted than, you know, sketchy, uh, products that head shops and gas stations.
Joe Moore: Mm-hmm. I think that’s really important for us to notice, like that the market is really doing weird things. Like I [00:38:00] saw all these mito brands recently, marketing product, like I’m all for product being out there and safe product especially, and especially if you’re advertising exactly what it is. Um, but you know, I think there were some brands that claimed years ago, Kyle, I don’t know if you remember this one.
Joe Moore: Um, they were claiming that. They were only selling functional mushroom brands and that, or functional mushrooms. And that some sort of counterfeit operation was actually selling use, leveraging their brand selling illicit product. Oh, wow. For a CO and, and, and OSI and, and things along those lines. And I, I think that was total bullshit.
Joe Moore: I think that was just kinda like what they were saying. Um, so they got in less trouble. But I think there’s, you know, there’s a lot there to how do we actually know what we’re buying is what it is. Um, are, is there accountability in the kind of chain of custody of the products? Generally in a illicit market, there isn’t.
Joe Moore: Um, and, uh, even in decrim, like in Colorado, like how do we know, like I think a lot of Colorado [00:39:00] brands are even doing the same thing. So, um, you know, work hard, work with each other to like, make sure it is what they say it is. Yeah. Test kits, like dance safe and, and whatnot can kind of test for some sy but I don’t know that they’re testing and differentiating with like four A-C-O-T-M-T and other things.
Joe Moore: So I wanna be really careful. That’s why I’m like excited about Reggie’s company, like Labs. Actually, did I tell you that story when someone, someone gave me a bar in San Francisco and I was like, I don’t know, I’m definitely not gonna eat that. And then I like looked at it later and like the lab logo was on it, Haifa Labs, like logo, all their trust.
Joe Moore: I feel more trust there. Yeah. And I was like, oh, actually I will assume this. Oh, fascinating. Um, you know, I obviously there’s room for like counterfeit and like some bullshit there. Yeah, totally. But better than, you know, a sketchy like. Uh, unknown kind of branding package with who knows what in it.
Kyle Buller: [00:40:00] Yeah.
Kyle Buller: Yeah. And I don’t know, like, like you might need to send some of those bars in for like mass spec, because I think picking some of this stuff is like really tough. I, I was on a website, I forget what it was called, like know your drugs.com or something like that. And they did have like, chocolate samples and they said it’s a little bit harder to kind of, uh, pull out, um, active compounds in some of the, um, some of the, like the, the chocolate bars and stuff like that.
Kyle Buller: ’cause there’s just so much stuff in it. But, um, I don’t know. I, I thought that was kind of interesting. Um, they had like little notes that, you know, like all the organic matters showing up and it’s hard to like, really tease apart everything when it comes to like those types of products.
Joe Moore: Right. It’s, I, I think really important to note, um.
Joe Moore: So just be careful out there. Um, what else has been interesting? I think it’s interesting, like, you know, so Santa Fe, we didn’t really get to talk about the Santa Fe conference. Um, there was yet again, a lot of activity from the Texas people in that like [00:41:00] overarching Iboga community. Um, and it was, it was interesting to see that momentum there.
Joe Moore: And then, um, Brian Hubbard getting some great stage time and then getting a lot of interest too. ’cause New Mexico deals with a lot of addiction. Um, it’s kind of clear that IGAs not purely for opioids at this point, which kind of used to be the label, but it seems to be helpful with all sorts of addiction.
Joe Moore: So I think there’s, there’s definitely some interest even in New Mexico around Ibogaine, which they haven’t really kind of gotten loud about yet, but that’s cool. Like Arizona put in money after Texas is 50 million. I heard rumor Mississippi might be Wow. Coming soon. Um. So it’d be really interesting for the US self to be kind of radically influencing, um, psychedelic and, and iboga policy.
Joe Moore: Um, should be fascinating.
Kyle Buller: Yeah. Was there any other like big insights away from that conference? It, I’m so bummed I didn’t get to go down there, but it was also a, just a good decision not to go. [00:42:00]
Joe Moore: Sometimes we need to rest, apparently. I, yeah. Um, so, uh, what I learned about Texas and how Texas actually funded that 50 million.
Joe Moore: Texas on occasion will have like a huge, um, surplus in revenue, in tax revenue from like oil. Um, so it was like a crazy amount of money in surplus that Texas had that year in tax revenue. So they were able to actually just grab a slice of that. Um, and I don’t, like in Colorado, sometimes we get refunds from the government, which, uh, was happening with early cannabis, but I think like, um.
Joe Moore: Texas just grabbed a chunk of that money that was surplus because of tax revenues from oil, and then were able to just allocate that. So I thought, um, potentially some of that money came from an opioid abatement fund, but that’s not the case. Um, Brian Hubbard’s still on a war path around like mm-hmm.
Joe Moore: Corruption in Kentucky around the opioid abatement fund money. Um, he, he kind of laid that all [00:43:00] out at South by Southwest. I don’t, I’ve not seen him lay it out elsewhere yet in detail, maybe on Rogan a while ago, but yeah. Have you seen him lay that out yet?
Kyle Buller: I don’t think so, no.
Joe Moore: He’s working hard to put people in jail Wow.
Joe Moore: Around federal, like, not federal, but state, state level corruption and like, um, people who are in like the pipeline to be pre and president in the near future and all this kind of fascinating stuff. Yeah. Um. So David’s asking a thing here about the industry needs to mature, but who starts? I feel like nobody’s asking for ingredients, like, you know?
Joe Moore: Yeah. Like, that’s a big deal. I think we need to, like, you’re, you’re probably gonna see that kind of stuff in like, uh, Southern California and San Francisco first. Um, like Venice Beach, I’m sure they’re like, you know, super, um, super expensive ingredients and product, um, and listing it all. And, um, eventually people with like, uh, celiac and, um, other [00:44:00] insensitivities can really, or not insensitivity sensitivities can be a little bit safer when consuming.
Joe Moore: So I think like, it’s coming, it’s coming. Um, you know, things, things that I find interesting are, um, if somebody’s getting injected with a substance, like how are they feeling safe about that? Um, in a ketamine clinic, that kind of makes sense because there’s like that whole clinical supply chain and we kind of trust that as Americans.
Joe Moore: Yeah. Or Westerners. And then, uh, but if you’re in some underground clinic and somebody’s got a needle for you, like that’s a really interesting roll of the dice. Um, and even if it’s a apparently legal clinic, like what is that kind of, what do you want to know about that before they inject you? And I think we don’t even know that, um, as a culture, like as a kind of psychedelic consumers.
Joe Moore: Like I, I’ve been hearing about people injecting five M me o in the underground. I’m just like, how are you sterilizing that? How are, like, what kind of water do you use? Like how are you even measuring [00:45:00] like, you know, 15 milligrams or whatever it is, or eight milligrams for that. So it’s really, really a curious landscape.
Joe Moore: And thankfully a lot of, I’m not hearing a about a lot of injuries from that. Are you? I
Kyle Buller: haven’t, no.
Joe Moore: Um, but you know, there’s always stuff that’s possible. Um,
Kyle Buller: yeah.
Joe Moore: I’m sure there’s a
Kyle Buller: lot of stuff that we just don’t hear about. Right? Like, I’m sure it’s happening, but just not coming on our radar. But, you know, I think Dave, to your question, like who starts?
Kyle Buller: And I think it just starts with you. It starts with all of us, um, to just be better, better educated, more informed. Asking people those questions, you know, like, I was just so damn curious. I walked in that shop and started like, asking questions, you know, it’s like maybe they were a little freaked out.
Kyle Buller: Maybe they thought it was like a narc or something. But, um, you know, and it also happened again, like I was in, I think it was like West Palm Beach, uh, into like another hemp shop. And this guy was trying to convince me that some [00:46:00] of those bars do contain Cy, but it’s completely legal. Um, and I’m like, SI’s not legal.
Kyle Buller: Like, and he was like, no, no, it is. And I’m like, you’re putting people at risk here by like being like that open, selling this stuff in public, especially in Florida, you know, it’s like mm-hmm. But just people aren’t educated about it. And, you know, I think it, it starts with us to try to learn, um, and, and ask, ask those questions when we do come across those products.
Joe Moore: Yeah, absolutely. I think, um, I was buying some cannabis edibles in Massachusetts a bunch of years ago, and, um, the person behind the counter was going nuts about how amazing it is that mushrooms are legal in North Carolina. And I was very nervous about that conversation for obvious reasons, like number one, that it’s not.
Joe Moore: And um, you know, I, I even corrected the person when I got up there. I was like, Hey man, that’s like really risky. That’s a really like high risk location for substance. And, [00:47:00] um, I couldn’t convince him and it was fascinating. It’s like they’re selling it so it’s legal. It’s like that A doesn’t even b
Kyle Buller: Yeah.
Kyle Buller: Um, like somebody has a very high risk tolerance and is like just Yeah. Skirting the law here and taking risk.
Joe Moore: Right. And I think, you know, there’s, um. There’s a certain level of like, what is the actual risk? Like we feel, right, our outside perspective is that there is like a really high risk, but also like how many shops are getting busted, how many people are going to jail or losing assets for it?
Joe Moore: And like, I think it’s pretty low probably. Yeah, I think like collectively they’re kind of making these judgment calls, like, um, and carrying things like Minocin product. Um, which is really interesting ’cause it’s not. Federally scheduled Minocin. Um, but Federal Analog Act is still there. Yeah. So ostensibly you could get busted federally and you know, apparently I heard, I learned yesterday that [00:48:00] some lawyers are really comfortable with the idea of defending that in court, which I’m like, how, how are you comfortable?
Joe Moore: Like, maybe it doesn’t get prosecuted as much. I don’t know. Right. I think, I think it doesn’t, like it would be, it’s like a really expensive thing to go to federal court to challenge that kind of thing. And I don’t know if you remember, like Sasha Shulgin had a lot of like really great testimony around, um, ’cause the law, the Federal Analog Act is something along the lines of, it needs to be substantially similar.
Joe Moore: And, and Sasha was just on stage saying that doesn’t mean anything. And from a legal perspective you have no ground. Mm-hmm. But it doesn’t necessarily mean that, um, things won’t progress in a difficult direction for you. Yeah. Yeah. So here’s, here’s a piece of news, um, founded on filter. I think I saw it a marijuana moment yesterday.
Joe Moore: But, um, the Alaska campaign to legalize psychedelics is gathering signatures finally. Amazing. So they kind of took [00:49:00] the next step, um, and they need to collect 35,000 signatures. So there’s a, a lot of activities required, I think after the conference that they had. Um, what was that called? Uh, maybe Northern Lights or something.
Joe Moore: Arctic Lights or something there. Arctic Lights. Yeah. Yeah. Like after that I think they got a lot of really good momentum. I, I really thought about going, but I just couldn’t like in good conscience go before Burning Man. That seemed like absurd. Um, but it sounded amazing. Everybody had a really great time, um, and, you know, got to educate Alaska in some really important ways.
Joe Moore: Um, yeah. And do you know much about what they’re doing there?
Kyle Buller: Just a little bit like when we saw them present down in Denver, um, and hearing about like the campaign and they were feeling really confident, um, about like getting those signatures and like their initial kind of like polling seemed, um, yeah, pretty positive that they would be able to, [00:50:00] to pass this.
Kyle Buller: So, um, fingers crossed, that’d be really amazing. Um, if they’re able to get all those signatures right. And it’s a, it’s a, it’s kind of like a legalization initiative,
Joe Moore: right? Right. Somewhat. Similar to Colorado and Oregon, um, but also like a little different, just kind of popping it up on screen here. I like this here.
Joe Moore: Traditional healers would also be protected for spiritual, or sorry, ceremonial spiritual or cultural use of plant medicines through legal exemptions to state laws. So I think that would be really, really excellent. Um, that’d be awesome. I think, uh, they’re lowering kind of the civil fine for public consumption to a hundred dollars to kind of make sense, I guess.
Joe Moore: Um, especially if you want to keep people safe. Uh, and they’re, um, yeah, so it says right here, yeah, they’re building off Colorado, which is great. Um, so I, I’m excited. I would really be excited to see how they’re gonna do it, [00:51:00] um, and, and roll it out and, um, see how they’re tracking to collecting those 35,000 signatures.
Joe Moore: Um, it’s a big job, but it’s important.
Kyle Buller: Yeah. What’s the total population in Alaska? Do you know?
Joe Moore: No.
Kyle Buller: I’m like, I wonder how much, like you said, 35,000. Yeah. I wonder how like that is compared to like the just main population. Yeah. Three
Joe Moore: quarters of a million. Hmm. So it’s a big proportion still. Yeah. You know, but you know, thankfully there’s only a handful of big cities that they could work on and bring it through.
Joe Moore: Yeah. Um, so yeah, I think it’s, um, it’s fascinating to see how this might shake out. Um, I’m excited. Um, so yeah, I, I heard, uh, from some other people in, um, New Mexico that there’s interest in other things beyond mushrooms too. Hmm. So, you know, feeling really [00:52:00] amazing about getting mushrooms through, like through the state process, the legislative process as opposed to like a voter ballot initiative.
Joe Moore: But then they’re like, oh. There’s all these other really amazing things that we could contribute too, and like how should we think about that? Like what do you think about that? Like it’s amazing that it’s happening in my book, but it’s also like, it’s complicated ’cause it feels
Kyle Buller: they’re doing it more kind of like in a behavioral health model, right?
Joe Moore: Um,
Joe Moore: like they’re not doing as robust decrim, if that’s what you mean. Is that what you meant? Meant there?
Kyle Buller: Yeah. Or like needing a, a diagnosis because they’re really trying to treat like mental health with, with their bill. Like I haven’t, but they can
Joe Moore: expand. They New Mexico can really expand the scope of it through adding conditions.
Joe Moore: Gotcha. So, you know, I was able to talk a bunch about chronic pain conditions and they were really excited about that. And, um, they’re actually, um, doing some [00:53:00] trials, I think in the near term with ketamine in group to help validate. Psilocybin ingroup for their stake care. Oh, sweet. Which would radically drop their clinical care costs.
Kyle Buller: Yeah. Which would be huge. Um, and when does like all this go online? Did they talk about like a rollout of like when they’ve got a date?
Joe Moore: It’s about two years from now. Okay. I think, think they said like December 27 or something like that. 2027. I could be wrong on that, but about two years. So similar to all the other project.
Joe Moore: Yeah. Yeah. Everybody else’s rollout dates. Yeah. Yeah. Um, yeah. And I think, oh, here’s another good one. Um, it looks like, um, other universities are picking up this, uh, traumatic brain injury conversation, which I think is, you know, long past due. Um, share my screen again here. If you’re watching, you can see it.
Joe Moore: Um. Uh, yeah, this tool is [00:54:00] interesting. Sometimes, sometimes it works amazing. Sometimes it does not. That’s not the right one. Come on. Um, but it looks like, uh, in British Columbia, they’re gonna start actually looking at Oh, amazing. Um, right. It’d be really cool. Um, and I think, uh, we’re gonna see all sorts of interesting stuff come from that.
Joe Moore: So I, you remember the Nolan Williams Ibogaine study that we’ve chatted about a bunch, right? Yeah. Where, yeah. Um, where I think a number of vets kind of took the, I think it was IBOGAINE and five M-E-O-D-M-T protocol, either at, uh, I think it was all at Beyond. No, that’s not right. Amio. Amio. And, um, I think it’s interesting they’re including five at this point, but the people just.
Joe Moore: Their brain imaging looked so much better at the end of the protocol, and this was done with Stanford, um, published highly. Dr. Nolan, Nolan Williams is like hyping it like crazy, but um, but yeah, now it [00:55:00] looks like there’s more interest in, um. Treating concussions and I had that big concussion a few years ago.
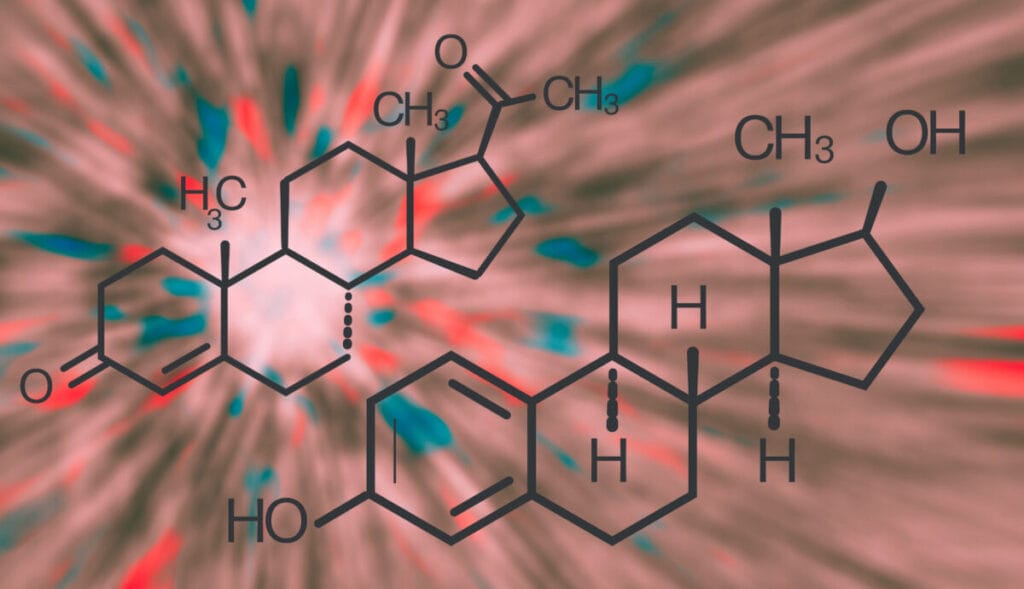
Joe Moore: Yeah. So I’m really, really excited about this. Um, yeah. Impaired neuroplasticity, so we know psychedelics can kind of help with that. Um, yeah. Reducing inflammation with classical psychedelics. Um, Chuck Nichols, Dave Nichols kid who’s like kind of an amazing researcher in his own right and is like wildly intelligent.
Joe Moore: Um, he’s kind of like the world leader on, uh, inflammation with psychedelics and he says psilocybin is a really good anti-inflammatory. LSD is a really crappy anti. Oh, interesting. Yeah. So like with the microdosing topic, it makes sense why some people have such a strong, well, from that perspective alone have such a strong response.
Joe Moore: And it could just be that it’s an anti-inflammatory thing.
Kyle Buller: That’s interesting. I wonder how much of an anti-inflammatory iboga is, or ibogaine, um.
Joe Moore: Right. Um, that would be a really interesting thing to know. [00:56:00] Yeah. Um, and I, one. Biggest things that ties into this is the, um, what are the molecules that are getting banned right now?
Joe Moore: God, um, uh, the DEA is working on these two really obscure molecules, um, Hamilton Morris and SSDP oh groups. Is it like
Kyle Buller: DOC or D-O-I-D-O-I-D-O-I
Joe Moore: and DOC. Thank you. Um, yeah. And these molecules, I think DOI in particular is showing like exponentially more anti-inflammatory response in people at a sub psychedelic dose than corticosteroids.
Joe Moore: So like a crazy high response rate. So if the DEA makes that illegal, um, or higher up the schedule chain, it makes it more expensive to research that stuff and, and not awesome. Um, but you know, imagine just people having to take less steroids. I think that would be just an overall good thing, right? Yeah, yeah.
Joe Moore: Totally.
Kyle Buller: Yeah. I’m excited for more of this like concussion [00:57:00] research to come out too. ’cause it’s like, yeah, you had your big experience a few years ago. Like I just had some minor, uh, head injuries over the summer. Um, and I was started to look up, um, some of this research and it didn’t seem like there was really great protocols.
Kyle Buller: Like some subjective reports came from people dosing. Like weeks after the concussion. And then, you know, I think there’s that question. It’s like, when do you start dosing? Do you start dosing as soon as possible? Do you, do you wait a little bit for the brain to kind of like, settle back down, um, and then, and then start dosing?
Kyle Buller: And so yeah, I was trying to do some research on it and it didn’t seem like there were very specific protocols around that. So I’m excited to, you know, uh, see more of that stuff. I mean, obviously being into some of these sports with, uh, high ri, high injury risk, you’re like, hmm. You know, like having concussions are not fun.
Kyle Buller: You know,
Joe Moore: I considered going into the thunderdome at Burning Man this year, and I think my [00:58:00] final conclusion was I don’t know that I can afford more brain injuries right now. Um, you know, I, so here’s, here’s a fun one. Um, and I’m gonna throw up and we can kind of like work towards closing two more. Um, where is it?
Joe Moore: Yeah, our friends, like we included these guys in our, um, TV show a while back. Yeah. Um, yeah, like, I don’t know that this is necessarily news, but they, they kind of showed up on our radar yesterday. Um, and they do this drug MEAI, um, and they’re bringing that through and that’s when it hits like a satiation trigger.
Joe Moore: And, um, I, it sounded like it had a really amazing, safe profile. It felt pleasant to use and it helped people stop drinking. And I think the article I saw the other day was around, um, overeating. And so if you hit, if you can eat this pill, um, it might help you just not overeat and, um, [00:59:00] similar to not over drink, you know?
Joe Moore: So I think that’s like a really cool idea and I’m excited to see what happens there. Um. Why is this psychedelic news? Um, what was the guy’s name? Mark Hayden, former Maps Canada lead was part of their team and I think he, he had some really interesting things to say about it. And it, I think the experience is something along the lines of, um, uh, how to put it,
Kyle Buller: I think they said low dose MDMA, like they said something like
Joe Moore: that.
Kyle Buller: Like when you’re using MEI for drinking, it was like you would feel satiated after like a drink or two. And then like, but if you took it alone and didn’t use it in combination, um, with drinking, they kind of described it as like a low dose of like MDMA.
Joe Moore: Mm. Yeah.
Kyle Buller: I think that’s fascinating. So, because I remember after all those interviews, I’m like, I kinda wanna try this stuff Sounds really fascinating.
Kyle Buller: Just for like, not for the drinking piece, but just for like the low dose of [01:00:00] MDMA.
Joe Moore: So Lindy is asking for us to link to a study. I don’t know. Um, which one, if you wanna look up Stanford Ibogaine brain injury. You’re gonna find that one if that’s the one we were talking about. Um, so this is like kinda the final bit of news we can leave folks with, but the Colorado Natural Medicine Board recommends iboga for therapeutic use.
Joe Moore: So it seems like the advisory board, um, that’s kind of contributing towards the government making its rules is saying Yes. IGAs. Next. I heard some inside stuff that it’s looking positive. I don’t want to give any details. Um, so I promised a little bit of an nomin and then, and then Jesus anonymity. Um, and check this out, it looks like, um, they’re really recommending compliance with the Nagoya protocol, which would be really novel and really good.
Joe Moore: Nagoya protocol is an international agreement, I think. Almost every country signed it except for the United States. So it’s like legally [01:01:00] required in other, in many other countries. Um, and, uh, as of right now, I think the only only known company that has Nagoya compliant IGA is, uh, AMBIO. They claim that pretty loudly and proudly, uh, um, but it, it could imp improve, increase the pressure on the markets to become more Nagoya compliant.
Joe Moore: So it’s kind of like built in reciprocity to genetic heritage. So like, do you have an agreement with the country and the, and the people from where this is from to say, yeah, like, you’re gonna give us a certain amount of your revenues? That feels fair. And you have it in writing and there’s, I looked it up on um, GPT the other day.
Joe Moore: There was a few other kind of like hit points for like, what is a Nagoya compliant agreement, but there’s no international authority that certifies it. There’s nobody that just like rubber stamps it, but there are like third party companies that kind of validate it. Yeah. Um, [01:02:00] so it’s an interesting thing to live with, uh, and live through, but I don’t know.
Joe Moore: Any thoughts on this one?
Kyle Buller: I was actually gonna ask you if you heard any updates on this. ’cause I did think, I just saw some posts about this and I didn’t really get to read into it ’cause I was, uh, teaching today. But, um, yeah, I mean it’s exciting. Uh, and it’s always like, I always find it like really interesting, like how IGA is getting like the spotlight right now.
Kyle Buller: ’cause you know, it is like one of the more on the riskier side, right? Of like cardiac issues. Um, so it’s fascinating like how much coverage and attention Iboga is getting and Iboga is getting. Um, but also really exciting ’cause it seems like the potential is huge. Um, here. So
Joe Moore: I like this quote from our friend Josh Cappel, uh, founding partner in Vicente.
Joe Moore: He says, unfortunately the program is not legal under federal law. Um, this is the Natural Medicine Health Act thing, like the psilocybin program and whatnot. Um, so it’s not legal under federal law, but there’s more than a zero chance that we can import iboga from [01:03:00] Gabon. Uh, Colorado would. The federal government to step in on this very nuanced, um, topic and authorize that, which is, you know, quite an interesting conversation to be having now.
Joe Moore: So, um, yeah. Yeah. Um,
Kyle Buller: yeah. And is it appropriate to like, grow Iboga here? Probably not. Or the climate’s probably
Joe Moore: not even great for it, but, right. ’cause it’s a rainforest that it grows in realistically. Are there other ways of doing it? That’s an interesting question. Like how can we do an end around on the federal law thing?
Joe Moore: That’s an interesting question. So there’s, um, yeah, there’s a lot, especially like if, if the primary objective is import is what’s illegal, bringing it from outside the country into Colorado is the illegal act. Um. Like possessing it still in Colorado is illegal under federal law, but you have state law protecting you, which is interesting.
Joe Moore: Right, right. Um, yeah, so it’s a whole fascinating legal situation that we’re dealing [01:04:00] with. And, um, there’s plenty of other fun, exciting, legal situations We’re also dealing with the same time, so who knows? Um, yeah. Yeah. Like all of a sudden IGA could be legal federally in two weeks who like, because it, you know, the,
Joe Moore: I don’t want to make too many dark comments, but Yeah. Like the science is there for all sorts of other things, and why isn’t it? Why isn’t it here for this? Yeah. Yeah. So, um, yeah. Anyway, uh, Lindy’s asking about the anti-inflammatory stuff. I don’t have the paper. Chuck Nichols, Charles Nichols, university of Louisiana is the researcher.
Joe Moore: Check out his papers. Um, he’s got a number of papers on anti-inflammatory effects of psychedelics. So a lot of good stuff there. And those drugs, um, D-O-I-D-O-C, they last too long. That’s why we don’t use them. Like, you know, if you wanna be like 24
Kyle Buller: hours or something like that, like the halflife is pretty ridiculous on it.
Joe Moore: Super high. Yeah. And if you wanna be high that long, just like, it’s probably more, far more [01:05:00] pleasant to just use acid for a couple times. Like, and you could turn it off like D-O-I-D-O-C, like good god. Like we just don’t use that stuff. But I’m excited to see what medicine can be made of that to help people who are in chronic pain and like, let’s see what, not only that kind of level of anti-inflammatory, anti-inflammatory stuff, um, happening, but pair that with neuroplasticity and what kind of change can we have.
Joe Moore: Mm-hmm. Maybe that’s what’s happening with high-dose mushrooms. Yeah. Yeah. Yeah. Cool. Well thanks for staying over with me and, um, yeah.
Kyle Buller: Thanks everybody for tuning in and doing this and yeah, it’s been quite a while since we’ve kind of, uh, riffed together, so it’s fun and hopefully we have, uh, more time to be doing this.
Kyle Buller: So
Joe Moore: yeah, let’s bring guests in to be like guest commentators too. Yeah, and again, please support us over@navigatorspsychedelicstoday.com slash navigators. We would love for you to be part of our community and support us and we can give you exclusive content and much more access to the, [01:06:00] um, you know, in-person events.
Joe Moore: We’ll be running and book club, film club and more so expect news. We’re gonna roll it out in phases. Um, but you can sign up now at our base membership level and we would love to see you in there. And, um, thank you Kyle.
Kyle Buller: Yeah, thank you Joe. And thank you everybody. Till next time.
Joe Moore: Yeah. Yeah.