Evelyn Eddy Shoop MSN, APRN, PMHNP-BC: Lived Experience, Qualitative Data, and the Future of Psychedelic Care
November 21, 2025
Overview
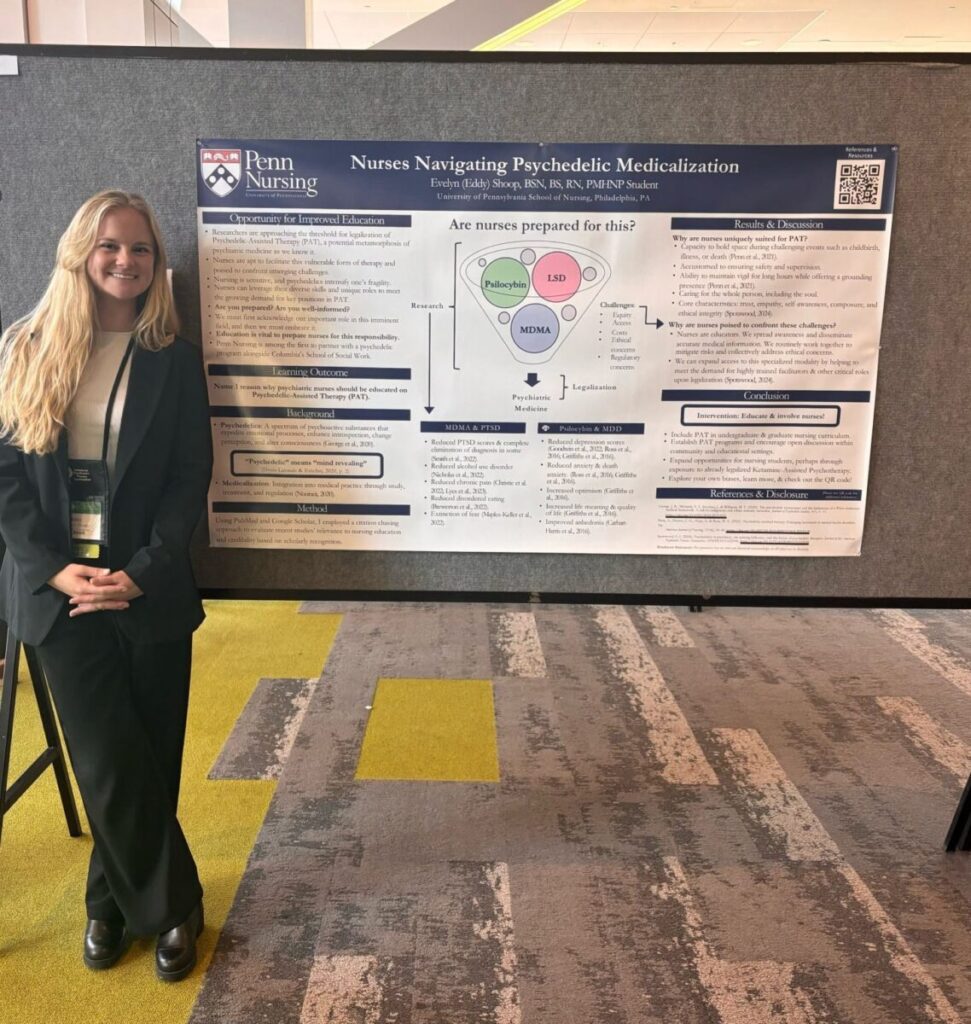
Evelyn Eddy Shoop PMHNP-BC joins Psychedelics Today to share her journey from Division I athlete to psychiatric mental health nurse practitioner and psilocybin research participant. In this conversation, she explains how sports injuries, OCD, and intensive treatment led her into psychiatry and eventually into a psilocybin clinical trial at Yale. Her story weaves together lived experience, clinical training, and a call for more humane systems of care and better qualitative data in psychedelic science.
Overview
Evelyn Eddy Shoop PMHNP-BC joins Psychedelics Today to share her journey from Division I athlete to psychiatric mental health nurse practitioner and psilocybin research participant. In this conversation, she explains how sports injuries, OCD, and intensive treatment led her into psychiatry and eventually into a psilocybin clinical trial at Yale. Her story weaves together lived experience, clinical training, and a call for more humane systems of care and better qualitative data in psychedelic science.
Early Themes: Injury, OCD, and Choosing Psychiatry
Early in the episode, Evelyn Eddy Shoop PMHNP-BC describes how multiple season ending injuries in college and serious mental health stressors in her family pushed her to rethink her life path. Originally pre vet, she stepped away from veterinary medicine after realizing she could not tolerate that environment.
During a semester off for surgery and mental health, she completed intensive outpatient treatment and family therapy. That time showed her how powerful psychological work could be. It also reawakened a long standing curiosity about the brain, consciousness, and human experience. This led her to switch her major to psychology and later pursue psychiatric mental health nurse practitioner training at the University of Pennsylvania.
At Penn, she felt supported academically and personally. Her interest in psychedelics grew as she realized that standard OCD treatments and high dose SSRIs were not giving her the level of functioning or happiness she knew was possible.
Core Insights: Psilocybin Trials, Qualitative Data, and Clinical Skepticism
In the middle of the episode, Eddy shares the story of finding a psilocybin trial on ClinicalTrials.gov just as she was about to start ketamine therapy. She received placebo first, then open label psilocybin, and describes the dosing day as one of the hardest days of her life, with benefits that emerged slowly over months through integration.
She uses her experience to highlight why qualitative data matters. Numbers alone cannot capture the depth of a psychedelic journey or the slow unfolding of meaning over time. She argues that subjective stories, even difficult ones, are essential for clinicians, researchers, and policymakers.
Key themes include:
- The central role of integration support in turning a crisis level session into lasting growth
- How trial environments on inpatient psychiatric units can feel like prison instead of healing spaces
- The limits of double blind placebo trials when participants become desperate for active treatment
- The need for more nuanced language around psychosis and psychedelic harms
Eddy also addresses skepticism in psychiatry. Many providers fear substance induced psychosis and feel uneasy with medicines whose mechanisms are not fully understood. She suggests that more lived experience stories and careful education can help bridge that gap.
Later Discussion and Takeaways
In the later part of the episode, Eddy and Joe discuss harm reduction, ketamine risks, and how poorly designed systems can create harm even when the medicine itself is helpful. Eddy describes being treated as “just another psych patient” once the research team left for the day, including being denied basic comforts like headache relief after an emotionally intense session.
She calls for:
- More humane hospital and research environments
- Required psychedelic education in psychiatric training
- Honest, nonjudgmental conversations about substance use with patients
- Stronger public education for students and festival communities
Eddy also invites listeners in Wilmington, Delaware and nearby regions to connect if they need a psychiatric mental health nurse practitioner for psychedelic related research. She hopes to bring her lived experience and clinical skills into the emerging field as psilocybin and other treatments move toward approval.
Frequently Asked Questions
Who is Evelyn Eddy Shoop PMHNP-BC?
She is a psychiatric mental health nurse practitioner trained at the University of Pennsylvania, a former Division I athlete, and a psilocybin trial participant who now advocates for more humane and data informed psychedelic care.
What did Eddy learn from her psilocybin clinical trial experience?
She learned that the hardest sessions can lead to deep change when integration support is strong and when there is time to unpack insights, rather than rushing to rate symptoms on a scale.
Why does she care so much about qualitative data in psychedelic research?
Eddy believes that numbers cannot capture the full human impact of psychedelic therapy. Stories show how people actually live with their disorders and integrate change, which is vital for ethical practice and policy.
How does she view psychedelic harms and psychosis risk?
She acknowledges real risks, especially for people with certain histories, but also notes that some psychotic experiences are not distressing. She calls for more precise language, better containers, and honest harm reduction education.
What role does a psychiatric nurse practitioner like Evelyn play in psychedelic care?
Practitioners like Evelyn can assess risk, prescribe within legal frameworks, provide preparation and integration, and help bridge the gap between traditional psychiatry and emerging psychedelic therapies.
Psychedelic care is evolving fast, and this episode shows why voices like Evelyn Eddy Shoop PMHNP-BC are essential in the current psychedelic resurgence. Her blend of lived experience, clinical training, and critical thinking points toward a future where data and story, safety and possibility, can finally grow together.
Links
Transcript
Joe Moore: [00:00:00] Hello everyone. Welcome back to Psychedelics today. I’m joined today by Eddie Shoop, nurse practitioner with a lot of other letters there. Really excited to have you today. Thanks for joining.
Eddy Shoop: Yeah, thanks for having me. This is a really cool opportunity. I appreciate it.
Joe Moore: Absolutely. I think it’s gonna be fun.
So. We got connected by the team at, the Penn Conference, Philadelic, which is gonna be, is that coming up in two weeks? Maybe? Do you know the date offhand?
Eddy Shoop: Yeah, November 22nd, I believe. Which is a Saturday.
Joe Moore: Yeah, so if you’re near Philadelphia, go check out that conference. It’s gonna be really cool. I went last year.
It was a, a little bit more expansive than what’s happening, um, on that day long event, but it looks like a really good day long event. I wish I was gonna be there for it. Um, and you know, there, I was told earlier today that the [00:01:00] focus of the conference will be iga, but it’s broader in scope than that, which is lovely.
Um, so can you tell us a little bit about what you’re hoping to present on there?
Eddy Shoop: Yeah, so, um, I will be on the patient panel and I think each person up there has about five minutes to talk about. Um, you know, their experience and what they’re hoping to, uh, project to the people listening. Um, and although I haven’t specifically curated exactly what I’m gonna say yet, um, it’ll be something along the lines of the fact that integration is.
Very, very important. Um, I don’t think that I would have been able to get as much as I got out of the study that I participated in if it weren’t for the support that I had throughout integration. Um, so I’ll probably touch on that and then, um, you know, just an opportunity to [00:02:00] share as, as someone who’s been through it, I think, um.
You know, there’s a lack of patient perspective out there, and we look a lot at the data and the numbers and things like that. But, um, it’ll be, it’ll be cool to share more of like the subjective experience of what goes on. So, yeah, that was kind of like a long-winded answer.
Joe Moore: Well, thank you for, thank you for that.
Could you give us a little bit, i of an idea of your background and, and how you ended up here interested in this topic? You know, I think worth noting as we talked about, uh, not to spoil you had some injuries, but you’re a big athlete for a while and then you kind of entered medicine. You kind of, that kind of arc.
Eddy Shoop: Oh my gosh. Yeah. What a question. So I, um, you know, growing up I played a lot of sports. I was very physical, um, and. That I, I would say that kind of became my [00:03:00] identity in a sense. And ended up going to the University of Florida. I got recruited to play lacrosse there, um, which was a tremendous opportunity.
And then I ended up having multiple, uh, season ending injuries. So that was definitely a lot to deal with. And at the same time, there was a lot of, um, mental health. Stressors going on in my life, not only personally, but with members of my immediate family. And at that time I was pre-vet, so I wanted to be a veterinarian ’cause I loved animals growing up.
But after working in a vet hospital as an intern for a couple of months, I realized that that was not for me because I couldn’t handle it. Um, and. There was one semester where I, I ended up taking the semester off, uh, not only for surgery but [00:04:00] for my own mental health. And that’s when, um, I kind of ended up doing like an intensive outpatient type of thing.
And after that I, I realized how. Like what I had been through in terms of, you know, learning through family therapy and all the things going on within my own family and then going through this long treatment process myself. And I was just learning so much and I realized. Since I was little, I had such an interest in the human brain and consciousness and all of these things, and it all kind of just came together.
And I almost had this like epiphany where I was like, I wanna like learn more about the brain. And so that’s when I chose, um, the psych psychiatric mental health nurse practitioner route. Um, and so I changed my major to psychology and. I finished school, finished college, um, [00:05:00] had to take a medical release because, you know, I ended up tearing my A-C-L-M-C-L meniscus and it was just a really nasty, nasty injury, so it wasn’t worth, um, playing again.
Um, and then, you know, but it was fine. ’cause then I got into Penn for nursing school and that was like. A huge wake up call for me because I had been so invested in sports. And then, um, you know, here I am, I’m, I’m capable of academic things as well. And so that was really rewarding. Um, and then, you know, Penn just was an environment where that I could really thrive in.
And I felt super supported throughout my whole education, um, at Penn. And that’s when my interest in psychedelics really kind of took off. Um, and although I had been through, uh. Treatment for my obsessive compulsive disorder, you know, throughout college, I felt that I wasn’t functioning as optimally as I could have been.
[00:06:00] You know, I wasn’t as happy as I, I felt like I could have been, and I was exploring ketamine and I was exploring, you know, going back on high dose SSRIs or, you know, diving back into like more intensive therapy. And I, I didn’t really know. What to do. And I knew that I was interested in psychedelics. So I, I went on, um, clinical trials.gov.
I sent a couple emails out to studies that were recruiting. And, um, it was actually on a Monday, I was about to do ketamine. I was about to start ketamine therapy. And then I got an email from the study recruiters and they said, Hey, we need a patient. Can you be here next week? And at this point I was, um. I was not quite in my master’s program, but I had a small period of time off and I made my way up to Yale School of Medicine for the trial.
And it was a very pivotal moment in my journey with my disorder, um, [00:07:00] in the most positive way. And so that’s just really reinforced my interest in psychedelics. And since that, um, I not only have made. Huge growth as a person and, um, in my own happiness and my relationship with myself. But, uh, yeah, I’ve also just really grown to, to wanna contribute to this field as much as I can.
Joe Moore: Well, I appreciate that it’s important and we have so many people contributing. It’s, um, the story I like to tell Eddie is that we’re. Many decades behind where we should be because of prohibition on, on the substances and prohibition of science. And we’ve really, really need to spend so much time and resources catching up to where we should have been on account of prohibition.
So, mm-hmm. So many basic questions. We have no [00:08:00] clue. Um, and I think, you know, I love, I love the title of the talk you gave at psychedelics beyond the Data because this, um. Or how do we say that? Psychedelic X. Psychedelic.
Eddy Shoop: Yeah. I, I go back and forth with it. I don’t really know.
Joe Moore: And, and that was kind of like a, like a student run conference, right?
Is that
Eddy Shoop: Yeah. Yeah. Uhhuh,
Joe Moore: yeah, they did, they did a good job on that. Um, so the idea is that there’s a lot of stories that aren’t captured. Somehow we’re, we’re kind of, um, not getting the whole picture when we just look at papers with a lot of numbers, right? Yeah,
Eddy Shoop: absolutely.
Joe Moore: Like we should look at those numbers and understand them, but, you know, how do you like to talk about this?
Eddy Shoop: Yeah, I mean, I, as someone who. Has been in school for a long time. Um, it, it can be easy to get wrapped up in the numbers and the science and the pharmacology and the mechanism of action. [00:09:00] And that’s all super important things to be talking about. But at the same time, when, when we’re speaking about these psychedelic compounds that are so powerful and that take your human experience outside of something that is of what we know on planet Earth.
You can’t break it down to numbers. Like you need some sort of subjective component where you can really hear what these people are going through because I, I really do believe that these self derived insights that are subjective are, that is the mechanism, at least for me, that was the mechanism of my healing.
Um
Joe Moore: hmm.
Eddy Shoop: So I, I would like to see more voices and people coming forward, even if their experiences are challenging and they don’t get something out of it, that’s also important. We need to hear, um, as much as we can from the individuals going through it. And I also know that it’s, it’s challenging to talk [00:10:00] about your own battles with mental health.
And so maybe that’s one of the reasons why, um, it can be difficult to hear people’s stories, but. I mean, if you’re someone that’s, that has something to say, I encourage you to, to speak up and, and let your voice be heard to the people doing research on this stuff. ’cause we need to hear it.
Joe Moore: Yeah. Um, absolutely.
We really do have a lot of, um, reason to thank people who came out about their stories, trusted. People with their health in these clinical trials. Um, people that really have been working in the underground for decades, just really not able to show their face or talk about their results or anything.
Mm-hmm. For fear of all sorts of retribution, so. Mm-hmm. Yeah. I think, yeah, there’s [00:11:00] so many stories yet to be told also, and yeah. Put in writing. Um, but yeah, I think, you know, stories supported by data are the best way to really communicate things. So, hey, here’s this data. Look at these three stories that kind of support this data.
Mm-hmm. And that’s how you really convince politicians and maybe even grant fund, uh, funding organizations that issue grants. Mm-hmm. Um, yeah. Have you, have you seen any success in any of those lines? Like, how do we actually get this research funded through, through story and data?
Eddy Shoop: Um, you know, I haven’t seen much.
I, I was at, um, the psychedelic Science conference and, you know, even there, I, I really dug to find. Presentations where people were talking about their own personal experience. And I found one, um, I think it was some US veterans were speaking about their [00:12:00] experiences with MDMA. And so I went to that and that was great, and I just, I wanted more of that because those are the things that stick with you and especially like from an academic perspective, I guess.
Um. When you see case studies, you know, they say you learn and practice, you learn when you remember a certain case with a patient. That’s how you learn, uh, best. You know, you can memorize and study and look at numbers all you want, but um, yeah, it’s those experiences that like stick with you and help you remember most.
So, yeah, I don’t know if I answered your question, but Yeah,
Joe Moore: for sure. You did great. Um, and. I wonder, um, how do, uh, let’s see. Sorry. Um, it’s okay. These, these drugs are so powerful and so interesting and just like, kind of transcend what we usually think medicine is like. We have this kind of talk track [00:13:00] about them achieving like curative results in psychiatry, which you don’t usually talk about.
Cures in psychiatry. Mm-hmm. Um. And, you know, none of these things are silver bullets, right? Like, it still requires a lot of work, um, not just the drug. Mm-hmm. It’s just that the drugs with the work can be really, really helpful, um, maybe beyond SSRIs. Yep. Um, in your, in your schooling, I assume you didn’t really talk about psychedelics a ton.
Like professors weren’t giving you weeks and weeks of psychedelic lectures.
Eddy Shoop: No, not weeks and weeks. But shout out to Anita Iyengar at University of Pennsylvania. She’s really doing a lot to, um, have more education about psychedelics in the field, in the school of nursing at Penn, which is great. Um, no specific.
Like modules on psychedelics while I was in school. But, um, you know, you can tell professors are starting to become more open. Uh, they, they can feel [00:14:00] this research kind of creeping up on them and they know that they’re training, uh, future practitioners that are gonna be practicing with medications that are FDA approved and.
Um, you know, we need to be prepared for when this happens. We don’t wanna be the ones playing catch up. And so, um, I think, I think they’re starting to recognize that and the professors at Penn are doing a great job, you know, trying to implement more education around this. But it’s just, it’s tricky when it’s not approved.
And so you also don’t wanna waste time taking away from tools that we already have that are approved. Um, so yeah.
Joe Moore: Yeah. Right on. I think, um, so many people are yearning for deep, deep education at university. There’s a couple projects Yeah. That are, um, coming in that should be helpful, but from what I understand, they’re not perfect.
You know, like it’s, it’s always gonna be an, an [00:15:00] ongoing developing thing, but just giving students access to this information, hopefully in a structured way, what do you need to know? Um. Mm-hmm. And then, you know, there’s always the edgy thing, like how do you actually allow, let’s see, how do you allow people to have experiences, you know?
Yeah. In the early days of LSD, like it was really common to give students LSD, so they could actually. Experience it in, in this like, um, psycho psychotomimetic framework where you’re like instantiating psychosis. Mm-hmm. So you can understand it better, maybe.
Ah,
right. Um, yeah, which is interesting. I don’t, I don’t know how I feel about that.
I think actually let’s, let’s get into a fun one real quick, and this, I think this goes into beyond the data a little bit. Okay. So I’ve been having debates here and there about psychosis. Like, mm-hmm. Psychosis is a really specific diagnosis. Right. But it’s a really, in that specif specificity, there’s a bit [00:16:00] of broadness.
So I wonder if it’s actually a super useful term for us to be using in the psychedelic landscape because Yeah. My sense is that there’s a, um. There’s a lot of categories of experience and mental states that could fall in that category that aren’t necessarily like, bad or harmful to the person. Mm-hmm.
And they could actually be therapeutic. Yeah. This is, this is a, this is a speculation clearly beyond the data. Yeah. So you’re
Eddy Shoop: saying for an individual with psychosis, um,
Joe Moore: so you’re under the influence of psychedelics.
Eddy Shoop: Mm-hmm.
Joe Moore: Theoretically, you could be diagnosed as being, having psychosis. Oh yeah. You know, um, is that necessarily a negative thing to fall into the diagnostic category of psychosis?
If you’re in the middle of a psychedelic experience and isn’t, isn’t it possible that there’s like [00:17:00] subcategories inside, like yet to be fleshed out categories of lived experience that that would help us have better language when we’re trying to talk about psychosis?
Eddy Shoop: Hmm. That’s really, really interesting.
I’ve never thought about that before. And the one thing that comes to mind is like, I have come across, across patients with schizophrenia who are psychotic, but they’re not in distress. And you know, they are voicing that this has never bothered them. I’ve been having these visions and these encounters with.
You know those beyond humanity since I was seven years old. And you know, I have a relationship with these abilities and you know, the medication feels like it’s suppressing it. And that is so interesting to me because, you know, we need to, we have to, for these people, we have to find a balance between feeling grounded [00:18:00] on earth, taking care of our body, being able to do ADLs, activities of daily living.
Sometimes the medication, you, you need to take it in order to get there, but at the same time, like not, um, taking away this as they call it, ability. So I think that’s really interesting. Um, and then, you know, another thing that comes to mind for me is if people start to say that they have taken psychedelics and therefore they understand.
Psychosis feels like that can also be dangerous because people with psychotic disorders are so heavily stigmatized. Um, and so we have, I, I, at least from my perspective, would want to be careful with, um, using that terminology, if that makes sense. But I think it’s a really interesting way to maybe even de-stigmatize the term.
As well. So I don’t know,
Joe Moore: that’s [00:19:00] kind of where I’m going in part. So like, if we look at this basic, you know, here’s, here’s like, you know, Google AI’s first response, right? Psychosis is defined as the mental state, which involves, um, loss of contact with reality, making it difficult to distinguish whether is real and what is not.
If that’s the fundamental baseline, like good God, like
Eddy Shoop: yeah.
Joe Moore: Yeah, that’s, you know, when is. It’s, it’s rare to not have that sometimes. Yeah. Sometimes we can also be in it for hours,
Eddy Shoop: you know? Yeah.
Joe Moore: Um,
Eddy Shoop: that’s really interesting.
Joe Moore: And I liked how you said like the people with schizophrenia, with psychosis that aren’t in distress, you know, I think that’s real.
Yeah. And that’s, that happens something that we need to like really carefully discuss.
Eddy Shoop: Absolutely. And oh my gosh. Yeah. Yeah, because you know, we see people that act not like us and we need to give them things that make them act more like us. And sometimes I think, you know, after you give them the medication, that’s when [00:20:00] those negative symptoms really come in and they’re, you know, it really blunts their affect and it makes ’em less engaged in the world.
And, you know, maybe if we didn’t give them the medication, yeah, they’re out of touch with reality, but are they experiencing a life that’s more worth living possibly. Um. And so that’s something I’ve come across in practice that has really kind of rubbed me in some ways that are uncomfortable. But, um, yeah, I don’t know.
Joe Moore: Yeah, and like I, so when I, I think this feeds into the psychedelic harms conversation that’s developing, and I’m glad it is. I, when I see people discussing it, I’m, this is the kind of stuff that comes up for me. I’m just like, oh, how do we do this? Well, I’m just like. I’m kind of like getting tight as I’m watching the conversation.
Oh gosh, guys like this. This needs more care than that. [00:21:00] Yeah. Um, and even in, in sometimes scientific papers, it’s hard to get that level of care because you have to be so specific with what you’re trying to say. Right. Yeah. Um, and yeah, I don’t like, so when we talk about the negative psychedelic experiences, we’re often saying, oh.
You became psychotic. It’s like, well, that’s not enough of a statement.
Eddy Shoop: Yeah, yeah, absolutely. For 20 minutes
Joe Moore: per day for two days, was that necessarily harmful and was it harmful because the container wasn’t appropriate? Mm-hmm. Um mm-hmm.
Eddy Shoop: For that
Joe Moore: potentiality, you know, or was it
Eddy Shoop: harmful because you didn’t have the support to unravel it afterwards?
Mm-hmm. Yeah. Mm-hmm.
Joe Moore: Exactly, and I think a lot of this comes from the drug war and us not having like the last 5, 6, 7 decades or whatever to like collectively sort this out. Mm-hmm. Yeah. And now we’re dealing with a lot of folks that have, you know, a lot [00:22:00] of stigma in themselves about drug harm.
Eddy Shoop: Mm-hmm.
Joe Moore: Yeah. Um, yeah. Have you been seeing any good progress in the psychedelic harms conversation?
Eddy Shoop: You know, I have to say I haven’t been as involved in those conversations as I wish that I was. Mm-hmm. Um, I think that a lot of the involvement I have is more on like the clinical side and the medicalization, um, just because of the nature of where my, like life path has taken me, I guess.
But, um mm-hmm. The harm reduction piece is something that I need to brush up on for sure.
Joe Moore: Yeah. It’s, um, yeah, it’s interesting. I, you know, well, let’s go with one that we can actually speak skillfully about, which is ketamine, right? Like there’s this whole kind of bladder issue, um, oh yeah. That can develop and that’s, it seems to be with a specific genotype, like where I don’t, I actually haven’t seen genotype, but there’s a [00:23:00] subcategory of people that have this problem maybe metabolize ketamine differently and, yeah.
Have you, have you seen this characterized at all? Anywhere?
Eddy Shoop: I haven’t, I have heard about it. I haven’t seen it in practice at all. Um, from what I know, it’s you, you have to be taking like, way more than what would be technically prescribed for ketamine assisted therapy. Right. And, and ish you would have to, uh, ish.
Okay.
Joe Moore: So there’s edge cases. So it’s, um, in the ketamine assisted psychotherapy space, it’s like if you start feeling pain. Stop taking it immediately, pain while peeing, immediately sees ketamine. Um, and that can happen sometimes in the first couple administrations. It’s rare. Um, but yeah, like when I hear of people that require surgery, they’re doing an incredible amount of ketamine pretty much daily and that’s, you know, clearly not a good idea.
Yeah. [00:24:00] And then there’s, yeah, I have one friend that did it maybe two or three times, and then he had problems peeing for four years. Oh wow. Yeah. So edge case, right? This is like one story. Yeah. Um, but you know, we’re seeing a lot of benefit from it, but also harm. Mm-hmm.
Eddy Shoop: Yeah. And that goes with anything, right?
Um. Yeah, I mean, think about cannabis. There’s people with cannabis use disorder, there’s people with cannabis induced psychosis, alcohol. I mean, what percentage of our population has alcohol use disorder or is functioning at as like a, you know, a functioning alcoholic and maybe not living their life in a way that could be.
Better, I don’t know.
Joe Moore: Right. More fulfilling, happier, whatever. Yeah. Less suffering. Um, right. And it’s a almost a government subsidized drug. Yeah. [00:25:00] Like government imposed monopoly. Mm-hmm. Um, yeah. So I think we do, we do really want to be careful about any of these substances. And I, there’s this funny conversation I, I bring in sometimes Eddie around like, how.
Uh, might be flat lining. Um, how do I, I can hear you. How this line? Yeah. Uh, in my brains. Oh,
Eddy Shoop: I thought you meant the audio was like coming.
Joe Moore: No, no. I failed on that one. It’s, well, here it is. Here it is. Got it. All right. I rebooted. So the idea is like, um. Any kind of drug administration potentially carries risks and benefits, potential harms, and then, yeah.
Um, a lot of people are like, everybody should just be sober, right? Mm-hmm. And that just doesn’t necessarily seem like a position that we can push, right? Yeah. Um, it, it’s not really a tenable [00:26:00] position. And so how do we actually educate people skillfully about. All sorts of substances to say, Hey, like here’s the risks and challenges you might face if you take these on.
Yeah. Um, and I, I kind of come from this position of like, yeah, it’d be really great if people could use less alcohol. Um, for a lot of reasons. It’s a really kind of harmful drug. Mm-hmm. Um, and people’s poor hearts when they take methamphetamines, good god. Hmm. Um, people aren’t really ever. Educated on the heart risk Yeah.
Of methamphetamines before they use it. Right? Yeah. Um, especially smoked. And I, and I wonder what kinda like benefit we would actually have, you know? ’cause clearly dare Did you have dare when you were growing up?
Eddy Shoop: No,
Joe Moore: I have learned about it though. It, yeah. Yeah. Drug is this, uh, drug awareness, resistance education?
I think it was, yeah. It made me very excited about PCP and LSD at a very young age. Um, still have not tried PCP, [00:27:00] um, but yeah, it’s just like, what a thing. Like I, I don’t think they gave us the real story. Yeah. Um, and I’m hopeful there. So. Are you, are you excited at Penn to connect with anybody in particular about what you plan to speak about?
Eddy Shoop: Yeah. Um, I’m excited to connect with all of the people at, uh, Penn Psychedelics Collaborative. They’ve done a really good job organizing this conference. Um, also Anita as well. She’s really been my mentor throughout all my education. Um. She’s, she’s created a lot of opportunities for me and, uh, I’m excited to see her.
That’ll be a comfort to, to see her face, hopefully, if she’s able to make it. Um, but really quick, back to the education piece that you were talking about. I do think that education right now is so important, [00:28:00] not only on the clinical side, but on the public side. And, um, I just, I like that you brought that up.
Um, and I’m wondering if you have any ideas for how to foster more education, you know, in, in academic settings. Obviously this podcast is a really good way to disperse education.
Joe Moore: Yeah, but let’s see, I have, you know, been at it for. Almost 10 years starting in May. Um, and, you know, our first product that we ever put together to try to pay the bills for podcasting.
Mm-hmm. Um, just for the hosting bills, which is, you know, not terrible amounts of money. It was a class for college kids to have an easier time. College kids can really get lost out there and sometimes there’s real harms and risks and, uh, we wanted to not only mitigate and educate about those harms and risks, but how do we actually help them have the best use of that risk?[00:29:00]
Eddy Shoop: Mm.
Joe Moore: You know, um, I was chatting with some people in the harm reduction risk reduction space recently about what IFS can psychedelics today put together a series that we can put out for free. Um, which we’ve done, you know, 750 episodes for free here. So, you know, it’s not nothing. Mm-hmm. It’s just, you know, is that really the solution to this?
Not really this answer. Yeah. But how do we create an education package? Um, that we can host here or schools could put in their learning management systems for students to say, okay, I’m gonna engage with these things, or, I’m curious about these things. What do I need to know so I can be safer? Um, and I think, you know, on one hand people are gonna be hesitant to say, oh, we can’t do that ’cause more people are gonna use drugs.
On the other hand, if we’re not educating, we’re gonna have to catch people in rehab, in hospitals, um, potentially more than we would if we actually educated because, you know, um, there’s this really great, uh, success [00:30:00] story. Eddie in uk uh, the group is called The Loop. Mm-hmm. And the loop was providing onsite.
Free drug checking. Um, anonymously and hospitalizations year over year, uh, dropped 80%.
Eddy Shoop: Wow.
Joe Moore: From a music festival. Like what a huge success. ’cause people would say, oh, this has that in it. I’m just gonna throw that out.
Eddy Shoop: Yeah.
Joe Moore: I don’t want that anymore. Kind of
Eddy Shoop: similar to fireside
Joe Moore: ish. Somewhat, yeah. You know, fireside, if you’re having a really hard time, you can choose to call them over.
Um, the ambulance. You know, um, which is, you know, it’s, it’s fraught. I dunno if you need the ambulance, you call the ambulance, but how do you know if you need the ambulance? Yeah. Um, yeah. So I think that’s a big open question. But yeah, the idea is you go to the festival, drop off your drugs, say, is this safe for me?
Based on your own analysis that they mm-hmm. The, the service, the loop just provides you the [00:31:00] data and you get to make an adult decision
Eddy Shoop: Wow. At that
Joe Moore: point. Right. That’s
Eddy Shoop: really smart. Yeah.
Joe Moore: And it’s effectively illegal here to do that.
Eddy Shoop: Right. Um,
Joe Moore: to provide that service based on the, um, the Biden Rave Act from a long time ago.
And I think it’s, um, yeah, people could like lose their property, a property seized, all that kind of fun stuff, um, if they, and not to mention, go to jail if they knowingly had drug use on site.
Eddy Shoop: Yeah.
Joe Moore: Um. So the tides are turning. Mm-hmm. University groups are now allowed to actually provide test kits to students.
Even seven, eight years ago that wasn’t really available, even at a place like uc, Boulder, which is mm-hmm. Tremendous amount of drug use. Um, I remember the Psychedelic Club of Boulder actually getting kind of threatened by the university for providing drug checking kits like by Dance Safe and other groups.
Because it put their federal funding at risk. Yeah. Nevermind the lives of [00:32:00] their students that Yeah. You know? Yeah. Theoretically have some responsibility to, um, yeah. So in terms of education, we need to, we need to have education that people are, it’s easy to access. They don’t get in trouble for accessing it.
Hopefully it doesn’t go on their record for accessing it. Mm-hmm. Um, and they can ask questions. Um, they, they have safe spaces that they can access to, to learn more. Mm-hmm. Um, yeah. There’s just so much there to Yeah. To unpack and I think, I think we can make a lot of difference, you know, if we start making good structured education available to folks.
I’m told there’s people interested in funding that stuff. So hit me up if anybody wants to fund that kind of thing, I’m happy to help keep people out of prison and, and hospital.
Eddy Shoop: Yeah.
Joe Moore: And on the right side of the dirt.
Eddy Shoop: Yeah, absolutely. And even requiring it in, um, [00:33:00] psychiatric education, I think would be a huge piece.
Joe Moore: Yeah. Um, right. Like how do, how do people like yourself speak skillfully to drug using populations? Yeah. And you know, I’m,
I’m a unique case, right? And I, if I have to go to somebody who’s practicing psychiatry or doctor prescribing psychiatric meds of any kind, I have to play a really specific game. Yeah. And it’s, um. And it’s not great to mm-hmm. Have to necessarily not tell the truth or lie or kind of not disclose that I know a reasonable amount about psychiatry at this point.
Yeah.
Um, in order to get the care I, I need or want. Mm-hmm. And it’s really, really troubling. But that’s me as a special case. But then about. A guy that, or you know, any, any patient that goes and maybe they go rave [00:34:00] once a month, eat MDMA once a month. How do you actually talk to ’em about being safe as opposed to saying, I’m only allowed to tell you not to do it.
Eddy Shoop: Yeah. Mm-hmm.
Joe Moore: I think in the same way we can say, Hey, what if you only drank once a month? Mm-hmm. Or once a week as opposed to every day, you know, and like kind of trying to actually do the thing that keeps them safe. Right. Did you, do you ever have any frameworks of ed education or how do you practice around, how do you practice around that kind of thing?
Eddy Shoop: Um, well it’s funny because when we do like a substance use assessment, say like, what, you know, do you, you use any substances, alcohol and marijuana? Pills, cocaine, benzodiazepines, psychedelics. You know, they don’t really teach us to ask about that one. Um, but I always make a point to ask about it because it could be an opportunity.
To not only maybe like help someone get more out of [00:35:00] that the next time they choose to do it, um, but also, you know, provide some education. Like do you have a history of schizophrenia in your family? Do you have, um, a history of bipolar mania and, you know, an opportunity to educate those individuals that you know.
I understand you want to do these to, to explore and to learn more about yourself, which is great, and you’re allowed to do that. But you also need to know that this could throw you into mania. This could throw you into psychosis, and we wanna make sure you’re safe and you have someone there with you, um, when you decide to use them.
So the same way that we give, um, education about the benzodiazepines that we’re prescribing. I think it’s important for them to be educated on psychedelics as well, especially with the outpour of study results and all these outcomes that we’re seeing. Um, I think people are seeing these results and they’re wanting to get their hands on them, and these are people that are maybe already taking SSRIs who are interested [00:36:00] in trying some MDMA to see if it may helps them feel better because the SSRI isn’t working.
And then, you know, there you risk serotonin syndrome. And so people need, patients need to know about this. Um, so,
Joe Moore: mm-hmm. So I want to transition a little bit into, um, this qualitative data conversation and like, what, why are we missing the boat capturing qualitative data in, in research and, um, yeah. Do you, do you have any kind of thoughts on why we’re.
Just not capturing that or doing a good job telling those stories.
Eddy Shoop: I have a perfect example actually. Let’s have it. ’cause So the study that I participated in, mm-hmm. It was a very, very challenging experience. It was probably the hardest day of my life. Mm-hmm. Um, I really didn’t [00:37:00] reap the benefits of. The dosing session until a couple of months afterwards, and it was a really like grueling process trying to figure out, you know, what the insights exactly were and how I’m going to apply that to my life.
And it was, you know, I was processing a lot and at the same time, um, you know, there, there they did offer to. Or they asked me if I would like to participate in the qualitative interview, which was like 45 minutes long. And at the time I wasn’t prepared to talk about it. I hadn’t even processed it myself yet.
Um, and so I think it would be beneficial, I mean, maybe in future research if possible, to, to give it some time before you ask people to speak about it. And then at the same time, you know, a number is a number. You write it down, it’s one number. But someone’s experience. That’s a whole lot of words, and that’s a whole lot of [00:38:00] room, and that’s a lot to read and it’s a lot to capture in, in the right way.
So I think that makes it also tricky to kind of display that in the literature. Um, but that’s why videos are cool and
Joe Moore: mm-hmm.
Eddy Shoop: Conferences are cool too.
Joe Moore: Right. If we look at how maps trains people and other groups train people, they’re actually playing a lot of video. And so maybe it’s not structured data that makes it into papers, right?
Mm-hmm. But it’s, it’s almost like sports, right? You’re playing the tape. Yeah. Like pause and like, here what you do here and you know, I, I find that interesting and, um, hopeful. Um, but yeah, couldn’t we do a lot better if we captured tens of thousands of qualitative data points?
Eddy Shoop: Mm-hmm. Mm-hmm. And come up, you know, figure out what the themes are, what are the different elements that are arising, where we see parallels, and how does that go hand in hand with one substance, with one music [00:39:00] playlist, with one disorder that we’re looking at.
Um, you know, I think we have a lot to learn in psychology and psychiatry as well. And this could be a potential avenue to really expand our understanding. Of different disorders. So
Joe Moore: would you think it’s, it’s a bit of an inoculation against this kind of current replication crisis in psychology?
Eddy Shoop: Mm. How do you mean?
Joe Moore: So having all of these stories, um. They’re always gonna be unique. You’re familiar with this kind of like rep replication crisis, right? Like mm-hmm. Say ah, well, okay. A lot of classic fundamental stories in psychology are told over and over and over again. And it turns out with a lot of these things, there’re, you know, one-off studies this, the results cannot be replicated.
Hmm. Um, and they’re, they’re foundational to how we want to think about psychology. So. Like the foundational ways we think about [00:40:00] psychology are based on science that can’t be replicated, therefore major issues. Yeah. So I think like potentially there’s some benefit to like having a huge data set of qualitative data that, you know, even if we can’t replicate the study, we at least have these things that we can look at.
Eddy Shoop: Mm-hmm. That
Joe Moore: hopefully are valuable. Yeah. And maybe we can have a, you know. Yeah, mine them for some sort of hopeful things in the future. Yeah,
Eddy Shoop: yeah, absolutely.
Joe Moore: Um, yeah. Uh, so in your, in your presentation, you talked a little bit about skepticism in psychiatry. Mm-hmm. Can you talk about what, what you were trying to get at there?
Eddy Shoop: Yeah. Um, I think that. Uh, there are a lot of psychiatric providers that are resistant to, um, the potential [00:41:00] here with psychedelics. And I think that that is a protective mechanism because, um, you know, we, we see really severe cases on inpatient psychiatric units where, um, people have substance use induced psychosis or.
You know, they, they have done LSD and it has triggered the onset of schizophrenia. And I think that’s scary. And this is also something new and new things are scary. And, um, yeah, I, I think it’s just a, it’s a field that’s like grounded in evidence and data and. Uh, right now it’s tricky because the, the, the pharmacological mechanism for how these compounds are working is not fully understood.
I mean, really need, we, we kind of have somewhat of an understanding of what SSRIs are doing. Like we know what [00:42:00] antipsychotics are doing, uh, mood stabilizers. We kind of understand what they’re doing at the pharmacological level. But, um, with psychedelics, it’s really kind of, we, we don’t know why these.
These hallucinations are happening and there’s no like clear diagram that’s showing you why this is making someone feel better. And so I think that, you know, it makes people skeptical, um, which is why I think it’s really important that we voice those subjective experiences too.
Joe Moore: There’s a recent conversation that’ll get raised at, um, the psychedelic Lived Experiences conference that’s coming up soon in the conversations about harms and risks to the placebo group. Mm-hmm. Um. I was chatting with a friend the other day about her experience receiving the placebo part as part of the MAPS trial and how hopeless that made them.
I was chatting with some friends about, [00:43:00] um, their, their time working at some big research groups like Hopkins or NYU and just how desperate people are to access these treatments, and it’s like their last hope and then they receive the placebo and some people will become suicidal. Right? Yeah. Have you ever, um.
IWI wonder about what kind of qualitative data we could pull from that kind of thing. That would be useful. Yeah. That would be, have you ever thought about the placebo groups at all? Like that? That would
Eddy Shoop: be really interesting. I actually did receive placebo, um, in my study and I came back to get the psilocybin open label.
But, um, yeah, for me that was definitely super disappointing. So I would be really interested to see, and. Yeah. I mean, in a way, does that demonstrate potential bias? Um, I don’t know.
Joe Moore: Well, let’s go into that. So in, in terms of like the placebo, people having such a negative response and knowing they didn’t get it, [00:44:00] and therefore impacting the data.
By knowing they didn’t get it. Yeah, absolutely. Like I think there’s so many methodological issues of science here in, in RCTs, double-blind RCTs, like I mm-hmm. I don’t know necessarily what’s better, but I do know that it seems as though we’re harming people by doing mm-hmm. Placebo RCTs. Yeah. Um, and, um, there could be better ways to do this research, you know?
Mm-hmm. Um, uh, that’s not. Using this methodology. I don’t it, it might be worse data, but it might be more ethical data or probably is more ethical data. Yeah. Especially if we’re dealing with really desperate populations, right?
Eddy Shoop: Mm-hmm. Absolutely. Yeah.
Joe Moore: So I’m curious to see what happens there.
Eddy Shoop: Yeah, me too.
Because this is really unlike anything the FDA has ever looked at before. Um, so yeah, hopefully. Hopefully we see [00:45:00] something change soon. Yeah,
Joe Moore: please, please, please, please. Yeah, like it doesn’t, it seem like it’s just purely compassionate to explore that a little bit more. Like why would we wanna just keep doing that and
Eddy Shoop: mm-hmm.
Joe Moore: Felt like maps was treated a little unfairly, though they could have done it a little better, but you know, if we’re looking at these large pharma companies, it’s not like these people have the right to go kind of run to the media about it.
Eddy Shoop: Yeah, exactly.
Joe Moore: Mm. Right. So, um, yeah, I’m What are you particularly excited about psilocybin, given that was what you received in your trial?
Eddy Shoop: Yes, I’m very excited about psilocybin. Um, I. I see so many people who, and you know, maybe I am biased because I did have an experience where I had tremendous benefit. [00:46:00] Um. But, you know, I do wish that other people could have that opportunity. Like I had, and I encounter patients that I want them to have that opportunity.
And I wanna see what it can do for them. Because they’re, they’ve been on six different SSRIs. They’re getting ECT, they tried TMS, they’re, you know, in the hospital just laying in bed. Like, yeah, I’m participating in groups, I’m taking my meds. Like, I’m still not happy. I’m still not enjoying my life. And it’s like, what is the root of that?
And, you know, I know. Potentially something that could maybe help get to the root of that, but it’s not, I can’t use it. It’s not available to them. And so that’s been really frustrating. But I am super excited about the potential of, um, how many people that’s, this can help. And uh, that’s really what’s driving my desire to, to wanna be more involved.
Yeah.
Joe Moore: What do you, um. For whatever reason, ECT always gets [00:47:00] me. Um, you know, clearly. So when we, all right, I, I’ve taken very few oaths in my life and there’s this like Hippocratic Oath concept, right? Yeah. Um, of like, you know, do you know harm as a general kind of concept, right? But like, you know, I, is that really the right, so I get caught on language often.
I wonder if I have a problem with language, but I’m like, all right, so we’re gonna do a, the, like a intervention. Mm-hmm. That, you know, there’s a, a robust set of side effects. Um, when, when are those considered harm? And like, how do we actually negotiate around that? Do no harm concept.
Eddy Shoop: Mm-hmm. You know,
Joe Moore: like if we’re, our job is to do interventions that are the right interventions for the right patient at the right time, but also like, you know.
Do the least amount of harm.
Eddy Shoop: Mm-hmm.
Joe Moore: Take, take risks that the client is okay with, you know? How do you, how do you guys talk about that as a, [00:48:00] coming from a non-clinician that’s just kind of recreational internet doctor? I’m not, yeah. I’m not like a, I have zero clinical training for real. Just been at this for a very long time.
Eddy Shoop: Yeah. I mean, um, from my perspective, I. I mean, I am still technically in training. I, I’m licensed, but um, I’m still under the guidance of supervision right now. But as an individual who will be practicing, um, by myself at some point, I think that I’m really going to value the patient’s voice and. What their preference is, whether or not they have, I mean, capacity always comes into play.
You know, someone may not have capacity, which means they don’t understand their diagnosis, they don’t understand that they have their diagnosis and they don’t understand the risk versus benefit of receiving treatment for their, their diagnosis. You know, someone that lacks those um, elements, maybe I have to make a decision for [00:49:00] them, um, in order to get them to a place where.
They’re better. But, um, someone that has capacity to any degree, I think deserves, um, a seat at the table in making a decision for their treatment. And I have encountered providers that, um. Maybe don’t give them a high enough seat at the table, quite frankly.
Joe Moore: Mm-hmm.
Eddy Shoop: Um, and they say, you know, this is what, this is the next option.
And in the back of my mind I’m thinking, you know, there’s actually other options that we haven’t really discussed. Um, so yeah, that’s just the way I think about it. Um, ’cause after all the, this person knows themselves better than you do. You know, you might know all the science and. All of the potential avenues for treatment.
But, uh, at the end of the day, you’ll never be inside that person’s mind and understand their experience and,
Joe Moore: mm-hmm.
Eddy Shoop: Yeah.
Joe Moore: Yeah. I, [00:50:00] what’s our phrase? You are the world’s foremost expert on you.
Eddy Shoop: Yeah.
Joe Moore: And like to, to suppose that somebody’s like, um, a bigger expert. It just doesn’t really seem great. Right. Um, yeah.
And how do we do a little bit better there? I, I wonder? I think, um, yeah. Humility, training of some kind, being part of this psychedelic training is a big deal. Mm-hmm. And, you know, just because you’ve had this experience and you’ve read this in the books and whatever, you know, it doesn’t mean this new person’s radical, not radically different from that training.
Eddy Shoop: Um. Yeah.
Joe Moore: Hmm. Um, so from your lived experience of going through a trial, did you, did you observe things that you thought could have been executed on better from a, say this [00:51:00] wasn’t a clinical trial, and say it was actually a treatment? Like, do you, do you see things that could have been done that were, would’ve been better?
Eddy Shoop: Oh.
Even despite the fact that, uh, the environment that I in, that I was in was not a pleasant one. Mm-hmm. I still, still got a lot out of this therapy. Um, but yeah, I mean, it, I, it was on an inpatient psychiatric unit, which means I have no access to my phone. You know, a lot of my belongings were confiscated from me.
Toiletries, um. You know, you can’t have certain clothing. You’re sleeping on the most uncomfortable bed. Uh, the windows in your room don’t open. You don’t have access to the blinds behind the rails on the window because this is how we treat psychiatric patients in the United [00:52:00] States. This is the environment that we put them in.
Um, you know, you can’t even have visitors. Visitors have to come at a very certain time and it has to be scheduled and, uh. And, and you know, nurses are overworked, especially nurses working on psychiatric units where they have to administer medications to people, uh, without their consent essentially. And that’s not a fun thing to do.
Um, so the environment that I was in, the, the research team was working within the entity of the hospital. And so when the research team was gone after 5:00 PM I’m just a psychiatric patient to them. Um, you know, after my, after my dosing day, I had probably one of the worst headaches I’ve ever had in my life because of how much I was crying.
Mm-hmm.
And I asked for Advil and that wasn’t on my medication list, so I couldn’t [00:53:00] get Advil because, sorry, you know, it’s, I’m the nurse, it’s not on your med list, I can’t give it to you. Um, and so that’s something I had to deal with. Um, you know, the food wasn’t good and this just, it gave me a window into what, like the way that we are treating people with mental health disorders that are being hospitalized for their mental health.
Um, and I just think there has to be a another way. There has to be another way. It is prison. And I know this sounds like really harsh, but. It is like we need to start calling it what it is. We need to change something about this because it’s not an environment that people can thrive in and you know, they can’t even use pens or pencils.
They can’t, I mean, one of my family members was hospitalized for psychiatric reasons and. They weren’t even allowed to have sheets on their bed. They had to sleep on the plastic because they were a risk to su of [00:54:00] suicide. They couldn’t even use a fork. They had to use a spoon to eat things that normally you would eat with a fork.
I mean, there just, um, there has to be another way. How is someone supposed to recover an environment like that? And you know, a lot of the time when it’s depression especially, you have to wait four to six weeks. For the SSRI to kick in and, you know, then you also have them sitting in this environment and it’s just babysitting practically.
Um, but I’m really, I’m getting side. I’m getting side railed. Um, but yeah, that could be different, the environment, but I mean, have it in nature something, anything that’s less sterile. Um, and I think I, I actually was the last patient or participant in that study, and they actually switched out from out of, because I think the one that I was in was phase one or phase two.
And so now they’ve entered I think maybe phase three. And so they’re in an outpatient setting. [00:55:00] So the participants are actually getting two doses now and they can go home afterwards, and it’s in like a nicer environment, which is great to hear. But um, that was probably the most challenging part about my experience that I would’ve liked to change.
Joe Moore: How this, this feels like a ridiculous question to ask, but I’ve been hearing. Some examples to the contrary in the wild lately, but how, how essential do you think it is to have somebody that’s really skilled in the room for you in terms of like a psychological support, psychotherapy, things along those lines?
Like I, I, I’ve been just hearing some really kind of crazy stories. People just being like, kind of next to left alone for the experience.
Eddy Shoop: Wow. Um, I, I think. I can only speak based on my own experience and what I would prefer. Mm-hmm. And, you know, everybody’s different. Some [00:56:00] people may have it within them to be able to trust themselves and be able to process these things on their own and, you know, they may have that strength.
Me personally, I don’t, uh, it was really important for me to have, um, my facilitators there with me who really understood me. On a deeper level, and they helped me feel comfortable and grounded me. And, you know, not only for the dosing day in and of itself, but for the months following, you know, when I was really struggling processing what I had just learned.
Um, I knew that I had those meetings with them to kind of unpack it, and that was really, really important. But at the same time, it’s, it’s very patient led. And they’re not really asking you many questions. You know, you kind of, the, the patient is, they’re just the bumpers and the patient is the bowling ball, bowling or whatever.
Mm-hmm. Um, so the, the person receiving the [00:57:00] therapy is really driving what happens and really the medicine is driving what happens. ’cause the person getting the therapy isn’t deciding what they’re, you know, the, we set intentions, but. It’s gonna teach you what you need to learn about yourself, not what you want to learn about yourself.
So I do think it’s important, um, for people who know their boundaries and know their limits. Um, but I mean, I’m sure there are people out there that can get benefit from it without having facilitators present as well, I would hope that they proceed with caution. ’cause you never know what could come up.
Joe Moore: Mm-hmm. Yeah. What, um, so at the very least, they should speak your language, right? Yeah,
Eddy Shoop: yeah.
Joe Moore: Yeah. Okay. Um, got it. So, but yeah, I think you’re right on all these counts, right? There’s so many ways to improve this stuff. I think, you know, we [00:58:00] shouldn’t necessarily be crazy critical of the clinical trials as they inform what we’re gonna see in practice.
Mm-hmm. But it is, it is really the case that sometimes stuff’s just done poorly, but we could do so much better. Yeah, we could do so much better and we can keep improving and you know, hopefully in time we’re gonna see just, you know, the data, the actual quantitative data actually improving over time. Um, mm-hmm.
And hopefully qualitative data too. Um, any kind of major thoughts you wanna leave us with or, or things for folks to think about as they’re kind of learning more about the space?
Eddy Shoop: I don’t think so. The only thing I can think of is if you are someone that lives anywhere near Wilmington, Delaware, and you need a nurse practitioner to facilitate some sort of research, um.
To, you know, you, if you need a, a psychiatric mental health nurse practitioner for anything involving psychedelics, please don’t hesitate to reach out to me. Um, you know, I’m looking for [00:59:00] opportunities nearby. I’m completing this fellowship, I’ll be done in a couple of months and hoping to dive into this field as soon as I can.
So that’s about it from me though.
Joe Moore: Well, Eddie, thank you so much for spending time with us here and I really. Wish you all the luck at Penn for Phil Delic sharing some lived experience and more connecting with the scene. It’s such a good event, such a good group. Um, definitely wish I was gonna be there and, uh, look forward to seeing you at future conferences.
Thank you so much.
Eddy Shoop: I really appreciate you having me.